Antenatal Care
Model Inputs \(\rightarrow\) Health System Parameters \(\rightarrow\) Antenatal care
Overview
Antenatal care (ANC) can be defined as care provided by skilled health-care professionals during pregnancy to ensure the best health conditions for both mother and baby, including: risk identification, prevention and management of pregnancy-related or concurrent diseases, and health education and health promotion.[1] ANC can reduce maternal (and perinatal) morbidity and mortality directly, through detection and treatment of pregnancy-related complications, and indirectly, through identification of pregnancies at higher risk of developing complications. In addition, ANC also provides an important opportunity to prevent and manage concurrent diseases which may contribute to indirect causes of maternal morbidity and mortality, such as HIV and malaria infections.[1] Previously, a minimum of four ANC visits was recommended. However, the WHO now recommends a minimum of eight ANC visits (or ‘contacts’) as the four-visit focused ANC model does not offer women adequate contact with health-care practitioners.[2]
Data
We analyzed DHS data on ANC attendance from 1,713,875 women from 264 surveys in 75 countries. Here we plot the mean number of ANC visits by year for each subgroup.
Anemia
It is estimated that about half of anemia in pregnant women is amenable to iron supplementation,[3] however, this may be quite variable and is likely much lower in malaria-endemic areas. The WHO recommends daily oral iron and folic acid supplementation with 30 mg to 60 mg of elemental iron and 400 \(\mu\)g folic acid.[1] In settings where anemia in pregnant women is a severe public health problem, a daily dose of 60 mg of elemental iron is preferred.[1] If a woman is diagnosed with anemia during pregnancy, her daily elemental iron should be increased to 120 mg until her Hb concentration rises to normal.[1] A WHO review of the literature finds that low-certainty evidence shows that daily iron supplementation may reduce the risk of anemia at term (Hb <100g/L at 37 weeks of gestation or later) (14 trials, 2199 women; RR: 0.30, 95% CI: 0.19-0.46) and severe postpartum anemia (Hb <80g/L) (8 trials, 1339 women; RR: 0.04, 95% CI: 0.01-0.28).[1] Low-certainty evidence also shows that daily iron supplementation may increase maternal Hb concentration at or near term (34 weeks of gestation or more) (19 trials, 3704 women; MD: 8.88 g/L higher, 95% CI: 6.96-10.8 g/L).[1]
Complication recognition
ANC provides a unique opportunity to educate women on how to recognize complications during pregnancy, delivery, and postpartum, and a number of studies have found a positive association between ANC visits and knowledge of obstetric danger signs. A study in Madagascar found that receiving information about danger signs at ANC was associated with better knowledge of danger signs during delivery, with an adjusted odds ratio of 1.50 (95% CI 0.90-2.49).[4] A study in Bangladesh found that the odds of being “well prepared” was six times (OR 5.98, 95% CI: 3.85-9.28) higher for women with four or more ANC visits, compared to women with none or one ANC visit.[5] A study in Ghana found that pregnant women learn about danger signs from a range of providers, and regular contact with formal providers typically coincided with increased knowledge of danger signs.[6] A study in India found that adequate prenatal care was associated with better knowledge regarding the danger signs of pregnancy, with an odds ratio of 2.72 (95% CI 1.03-7.16).[7] Another study assessing birth preparedness and complication readiness found an odds ratio for 4+ ANC visits of 2.4 (95% CI 0.83-6.96).[8] In Tanzania, studies controlling for confounding and clustering effects found an AOR of 4+ ANC visits of 1.94 (95% CI 1.17-3.21) for birth preparedness and complication readiness,[9] and 1.4 (95% CI 1.1-1.9) for awareness of danger signs of obstetric complications.[10]
Parameters
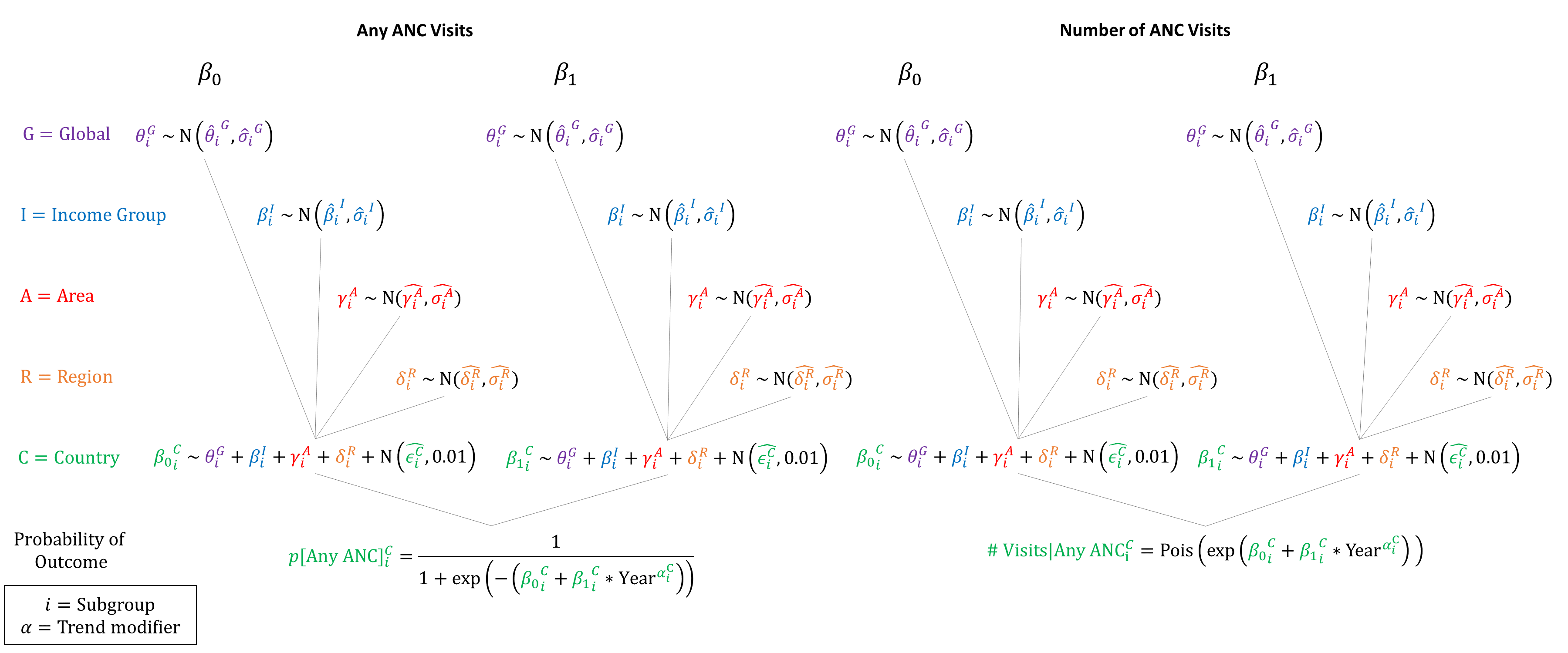
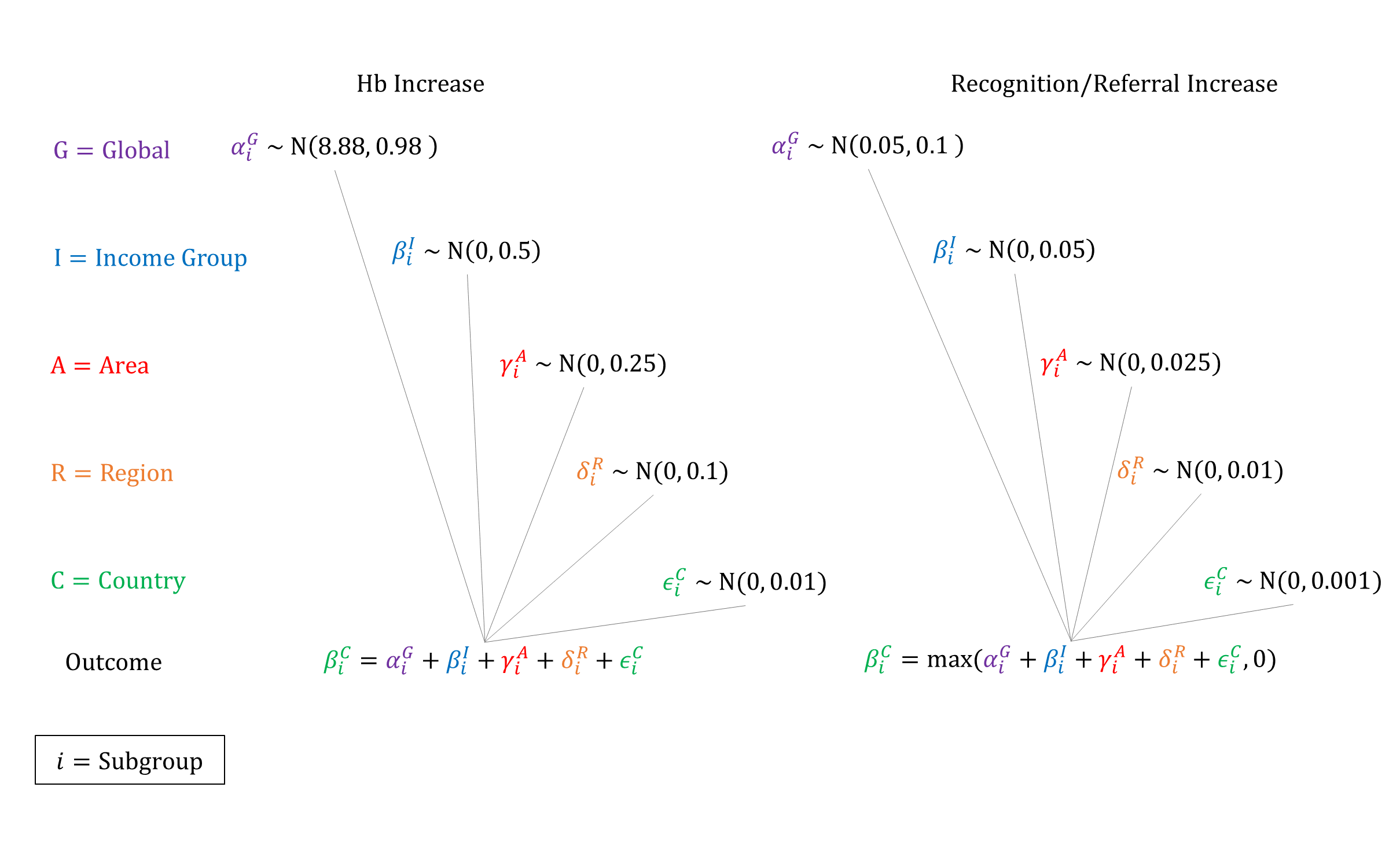
We used a two-part hierarchical Poisson model to estimate the number of ANC visits based on DHS data. We used upper middle income priors for high income countries due to lack of DHS data in high income countries. We also model the impact of ANC visits on anemia prevalence via an improvement in Hb concentration. We set priors based on WHO estimates that daily iron supplementation increases Hb concentration by 8.88 g/L (95% CI 6.96-10.80), assuming a linear relationship between number of ANC visits and and probability/efficacy of iron supplementation. Given that the mean number of ANC visits reported in the DHS data was 5.4, we re-scaled the Hb increase to be per ANC visit when sampling in the model. To model the impact of ANC visits on the probability of recognizing a complication, we set priors for a coefficient per ANC visit that is added to the hierarchical logistic regression model of recognition/referral. We assume that ANC only improves recognition/referral for women delivering at Home.
Priors
Model Implementation
The number of ANC visits is sampled at the beginning of each woman’s pregnancy. Based on her number of ANC visits, her hemoglobin concentration is adjusted and anemia status re-evaluated. Because the priors for anemia status are based on DHS data that include women who attended ANC, model calibration is used to lower the ‘natural history’ (i.e. without ANC) hemoglobin concentrations for women so that the distribution of anemia prevalence after accounting for current ANC coverage is similar to the observed DHS data.
References
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. 2016. Available at: http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf
- World Health Organization. WHO recommendation on antenatal care contact schedules. 2018. Available at: https://extranet.who.int/rhl/topics/improving-health-system-performance/who-recommendation-antenatal-care-contact-schedules
- World Health Organization. The global prevalence of anaemia in 2011. 2015. Available at: http://apps.who.int/iris/bitstream/10665/177094/1/9789241564960_eng.pdf
- Salem A, Lacour O, Scaringella S, et al. Cross-sectional survey of knowledge of obstetric danger signs among women in rural Madagascar. BMC Pregnancy Childbirth 2018; 18(1): 46. DOI: https://doi.org/10.1186/s12884-018-1664-x
- Pervin J, Nu UT, Rahman AMQ, et al. Level and determinants of birth preparedness and complication readiness among pregnant women: A cross sectional study in a rural area in Bangladesh. PLoS One 2018; 13(12): e0209076. DOI: https://doi.org/10.1371/journal.pone.0209076
- Aborigo RA, Moyer CA, Gupta M, et al. Obstetric danger signs and factors affecting health seeking behaviour among the Kassena-Nankani of Northern Ghana: a qualitative study. Afr J Reprod Health 2014; 18(3): 78-86. PMID: https://pubmed.ncbi.nlm.nih.gov/25438512/
- Gopalakrishnan S, Eashwar VMA, Muthulakshmi M. Health-seeking behaviour among antenatal and postnatal rural women in Kancheepuram District of Tamil Nadu: A cross-sectional Study. J Family Med Prim Care 2019; 8(3): 1035-1042. DOI: https://doi.org/10.4103/jfmpc.jfmpc_323_18
- Akshaya KM, Shivalli S. Birth preparedness and complication readiness among the women beneficiaries of selected rural primary health centers of Dakshina Kannada district, Karnataka, India. PLoS One 2017; 12(8): e0183739. DOI: https://doi.org/10.1371/journal.pone.0183739
- Bintabara D, Mohamed MA, Mghamba J, Wasswa P, Mpembeni RNM. Birth preparedness and complication readiness among recently delivered women in chamwino district, central Tanzania: a cross sectional study. Reprod Health 2015; 12: 44. DOI: https://doi.org/10.1186/s12978-015-0041-8
- Pembe AB, Urassa DP, Carlstedt A, Lindmark G, Nyström L, Darj E. Rural Tanzanian women’s awareness of danger signs of obstetric complications. BMC Pregnancy Childbirth 2009; 9: 12. DOI: https://doi.org/10.1186/1471-2393-9-12
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu