Referral Facility
Model Inputs \(\rightarrow\) Health System Parameters \(\rightarrow\) Referral Facility
Overview
Once transportation is arranged, a target referral facility must also be chosen. When referral networks are well-established, or in cases with good communication links with facilities, women can be taken to a facility that is able to provide the appropriate level of care. However, sometimes women are taken to multiple places in an attempt to find a facility capable of treating them. The selection of an inappropriate referral facility can be another barrier to receiving the care that is needed.
Data
A study in Malindi, Kenya, found that a majority of the women from rural areas seeking care first went to a dispensary or health center, from which they were referred to the district hospital.[1] In India, women who reported an obstetric complication in the Coverage Evaluation Survey (2009-10) were asked about the source of treatment they received. Most women consulted private doctors (54%), followed by government doctors (29%) and PHC (8%).[2] A study of over 1,000 mothers at 96 facilities found that most came directly from home, while 9.4% were referred from another facility.[3] Of the mothers who arrived at the study facilities, 6% were referred on for higher care. Tertiary level facilities were found to receive the most referrals, while secondary level facilities received very few referrals at all. In all, 12% of mothers who had been referred once required a further referral, half of whom went on to a private facility. In general, secondary level facilities were the common senders and tertiary level facilities were the common receivers. About half of referrals from primary level were sent directly to the tertiary level. Another study revealed that some women bypassed non-functional BEmOCs to seek care in higher-level facilities offering caesarean section services.[4] Bypassing primary care facilities to seek care in higher level facilities indicates that perceived poor quality of care may be an important determinant for bypassing behavior. If already at a facility, women can also experience ‘horizontal transfer’, meaning that they are referred to another facility that is similar to their current site. For example, a study of maternal deaths in India found that 25% of women referred were taken to 1 facility, 32% to 2 facilities, and 25% taken to three facilities.[5] (The remaining 19% did not reach any facility before death.) The mean time to make arrangements for travel from home to the first facility was 3.1 hours, from facility 1 to 2 was 9.9 hours, and from facility 2 to facility 3 was 3.1 hours.[5]
Parameters
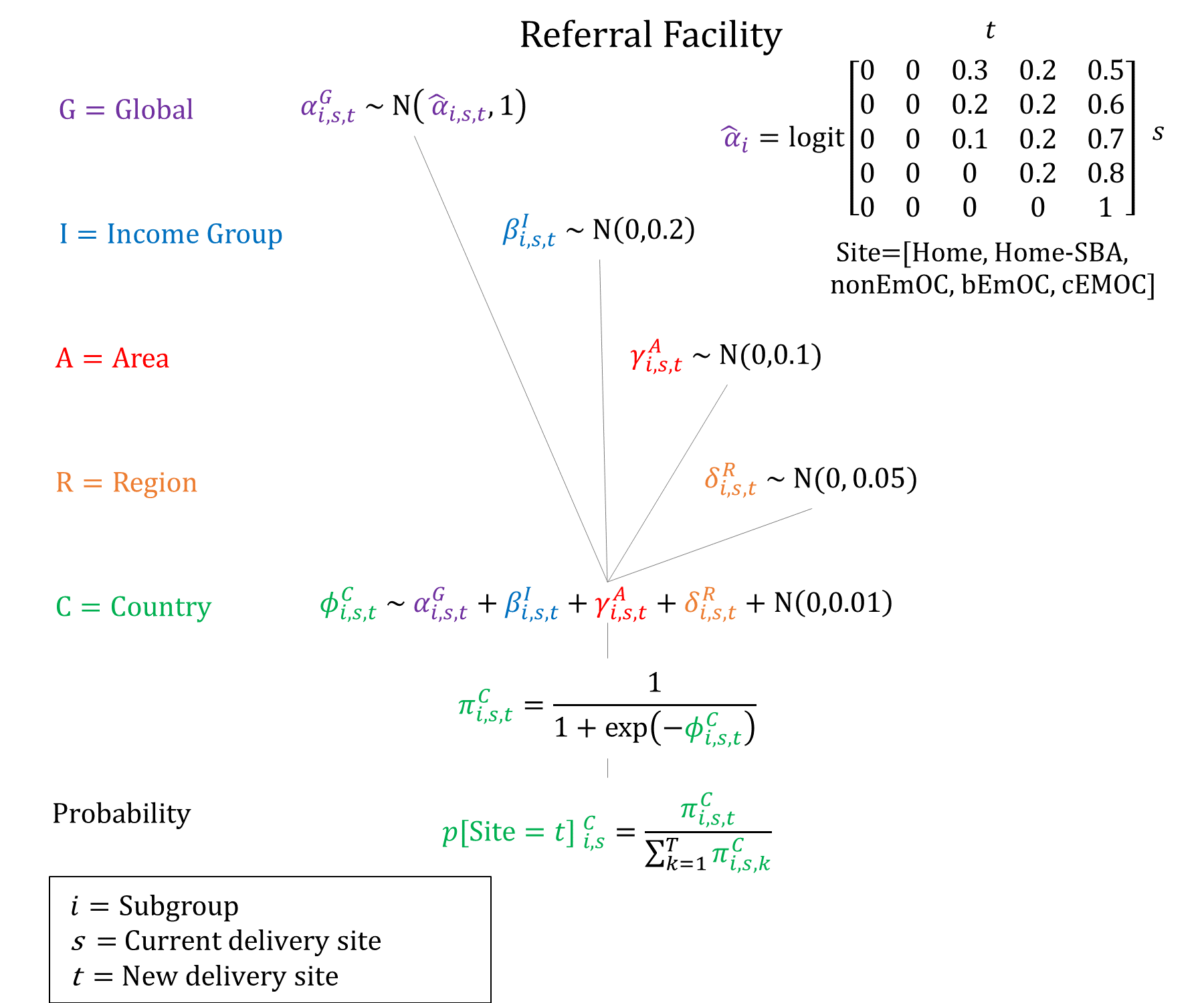
Given the preference for quality of care as seen by women bypassing lower-level facilities, we assume that referrals to CEmOC facilities are more common when setting priors.
Priors
Model Implementation
If transport is available, the final referral facility is simulated conditional on the current site. We assume that women in BEmOC are not referred to non-EmOC facilities.
References
- Echoka E, Makokha A, Dubourg D, Kombe Y, Nyandieka L, Byskov J. Barriers to emergency obstetric care services: accounts of survivors of life threatening obstetric complications in Malindi District, Kenya. Pan Afr Med J 2014; 17 Suppl 1(Suppl 1): 4. DOI: https://doi.org/10.11694/pamj.supp.2014.17.1.3042
- India Coverage Evaluation Survey 2009-2010. Ministry of Health and Family Welfare (India), ORG Centre for Social Research (ORG CSR), United Nations Children’s Fund (UNICEF). Available: http://ghdx.healthdata.org/record/india-coverage-evaluation-survey-2009-2010.
- Chaturvedi S, Randive B, Diwan V, De Costa A. Quality of obstetric referral services in India’s JSY cash transfer programme for institutional births: a study from Madhya Pradesh province. PLoS One 2014; 9(5): e96773. DOI: https://doi.org/10.1371/journal.pone.0096773
- Sabde Y, De Costa A, Diwan V. A spatial analysis to study access to emergency obstetric transport services under the public private “Janani Express Yojana” program in two districts of Madhya Pradesh, India. Reprod Health 2014; 11: 57. DOI: https://doi.org/10.1186/1742-4755-11-57
- Raj SS, Manthri S, Sahoo PK. Emergency referral transport for maternal complication: lessons from the community based maternal deaths audits in Unnao district, Uttar Pradesh, India. Int J Health Policy Manag 2015; 4(2): 99-106. DOI: https://doi.org/10.15171/ijhpm.2015.14
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu