Quality of Care
Model Inputs \(\rightarrow\) Health System Parameters \(\rightarrow\) Quality of Care
Overview
To account for health-system and facility-level factors not explicitly included in the model we include a parameter for ‘quality of care’, which has been defined as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge”.[1]
Real-world maternal health interventions have highlighted quality of care as an important determinant of outcomes, independent of facility delivery and complication referrals. For example, Janani Suraksha Yojana (JSY), a conditional cash-transfer program to incentivize facility delivery in India, succeeded in substantially increasing facility births, but had no significant effect on mortality due to lack of focus on the quality of facilities.[2,3]
We therefore include this parameter in the model to account for residual differences in maternal mortality not explained by differences in the incidence of obstetric complications and availability or efficacy of clinical interventions. Although it is a broad concept, the Institute of Medicine has described ‘quality of care’ as having six key features: care that is safe, effective, patient-centered, efficient, timely, and equitable. Although all these features are important, there are often particularly substantial deficiencies regarding patient safety (e.g., iatrogenic harm), effectiveness (e.g., providers may fail to provide the appropriate treatment even if it is available), and patient-centeredness (e.g., patients may opt out of or not adhere to treatment if they lack confidence in the health system).[3]
Parameters
We assume that quality improves by delivery site (Home < Home SBA < non-EmOC < BEmOC < CEmOC) and by income group. For example, we assume that higher-level facilities will generally have better-trained staff, such that interventions available in both BEmOC and CEmOC settings are expected to be delivered with higher quality in CEmOC facilities. We also assume that quality improves over time, and constrain the slope parameter to be non-negative when sampling.
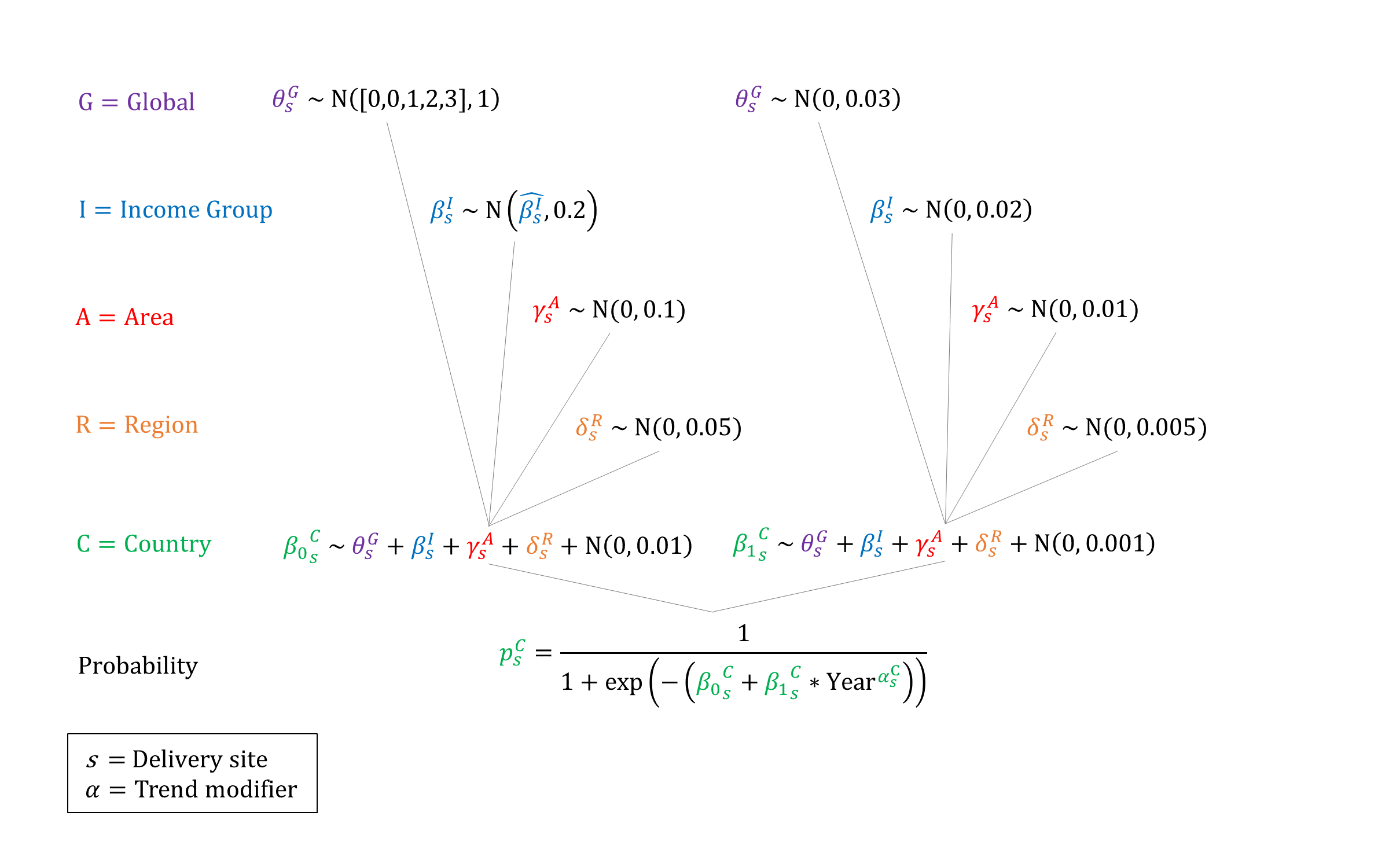
Priors
Model Implementation
The estimated quality of care at each delivery site is used to modify the efficacy of clinical interventions that may be delivered.
References
- Institute of Medicine. Medicare: a strategy for quality assurance. Washington, DC: National Academy Press, 1990. Available at: https://www.ncbi.nlm.nih.gov/books/NBK235462/
- Randive B, Diwan V, De Costa A. India’s conditional cash transfer program (the JSY) to promote institutional birth: is there an association between institutional birth proportion and maternal mortality? PLoS One 2013; 8(6): e67452. DOI: https://doi.org/10.1371/journal.pone.0067452
- Scott KW, Jha AK. Putting quality on the global health agenda. N Engl J Med 2014; 371: 1. DOI: https://doi.org/10.1056/nejmp1402157
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu