Antibiotics
Model Inputs \(\rightarrow\) Clinical Interventions \(\rightarrow\) Antibiotics
Overview
The mainstay of treating maternal sepsis is antibiotics, and we model the use of antibiotics in response to infection, rather than as a preventive measure. A Cochrane review found that while data are scarce, prophylactic antibiotics appear to be effective in reducing ill-health caused by infections in women who undergo operative vaginal delivery.[1] While the use of antibiotics for women undergoing caesarean section was found to reduce the occurrence of infection,[2] we assume that they are part of routine care for C-sections, and so do not explicitly model the use of prophylactic antibiotics. With the sharp decrease in maternal morbidity observed with the introduction of the antibiotic era, it is now accepted that antibiotic treatment is warranted for postpartum infection.[3]
Data
A Cochrane review evaluated the comparative efficacy and side effects of different antibiotic regimens for postpartum endometritis, finding that intravenous clindamycin plus gentamicin is more effective than other antibiotics or combinations of antibiotics for treatment of womb infection after childbirth.[3] While we could not find empirical estimates of the impact of antibiotic treatment on maternal mortality compared to no treatment, a previous modelling study assumed a case fatality rate for sepsis of 17% without antibiotics vs 2.1% if antibiotics are taken, implying an efficacy of nearly 90% on reducing mortality, although the authors acknowledged that these parameters were the most difficult to estimate.[4]
Parameters
For women who develop sepsis, we model the availability and efficacy of antibiotic treatment, conditional on delivery site. We assume that the availability of treatment increases by site and income group, and that treatment is not available at home. We assume that the efficacy of treatment is non-differential by severity, and apply the same risk reduction for all mortality and morbidity outcomes. We set efficacy priors centered near 90%.
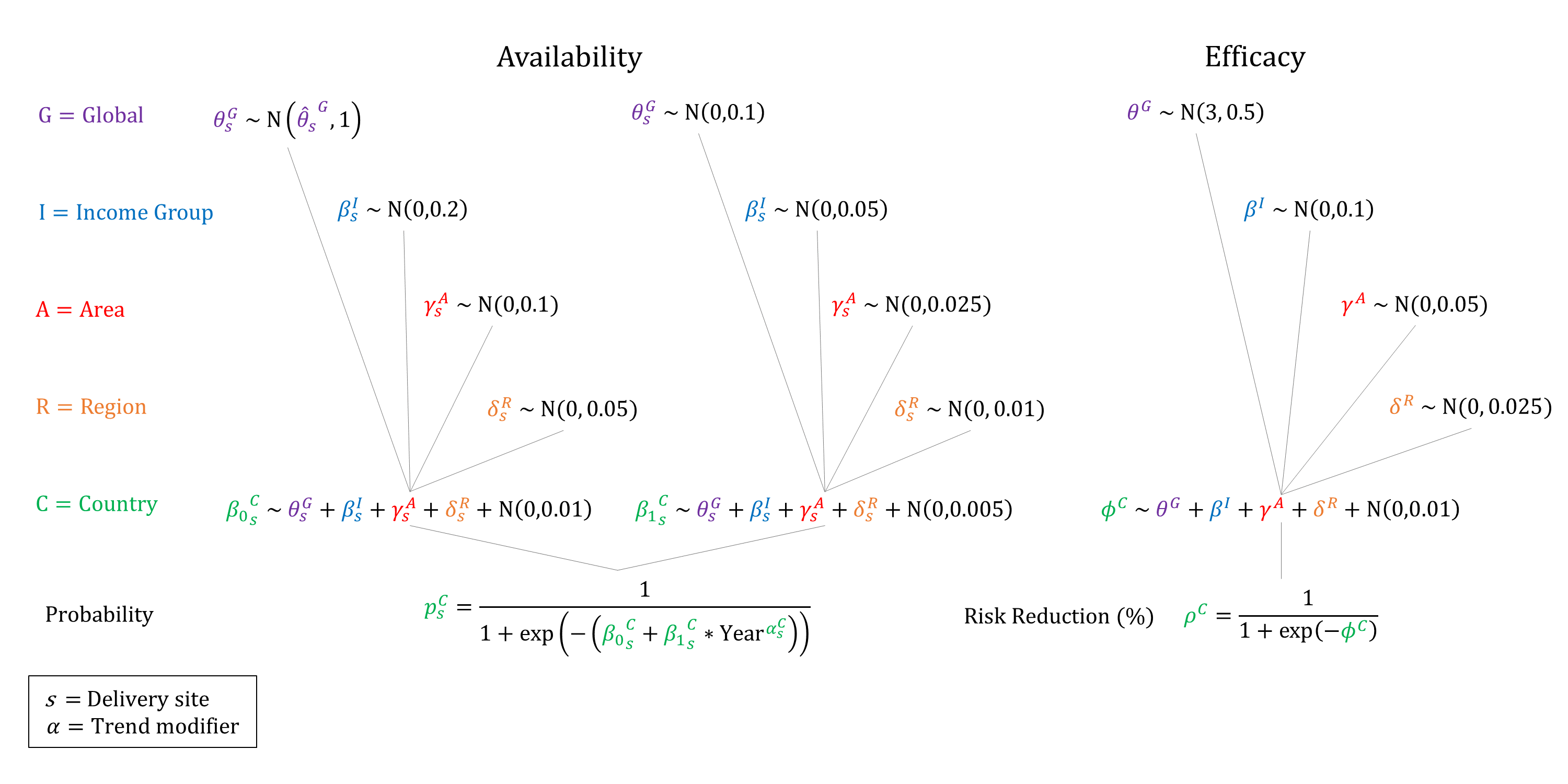
Priors
Model Implementation
Conditional on the delivery site we simulate the probabilities that treatment will be available and the efficacy of treatment on sepsis outcomes, accounting for quality of care.
References
- Liabsuetrakul T, Choobun T, Peeyananjarassri K, Islam QM. Antibiotic prophylaxis for operative vaginal delivery. Cochrane Database Syst Rev 2020; 3(3): CD004455. DOI: https://doi.org/10.1002/14651858.cd004455.pub5
- Smaill FM, Grivell RM. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database Syst Rev 2014; 10: CD007482. DOI: https://doi.org/10.1002/14651858.cd007482.pub3
- Mackeen AD, Packard RE, Ota E, Speer L. Antibiotic regimens for postpartum endometritis. Cochrane Database Syst Rev 2015; 2: CD001067. DOI: https://doi.org/10.1002/14651858.cd001067.pub3
- Pagel C, Lewycka S, Colbourn T, et al. Estimation of potential effects of improved community-based drug provision, to augment health-facility strengthening, on maternal mortality due to post-partum haemorrhage and sepsis in sub-Saharan Africa: an equity-effectiveness model. Lancet 2009; 374(9699): 1441-8. DOI: https://doi.org/10.1016/s0140-6736(09)61566-x
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu