Lactational Amenorrhea (LAM)
Model Inputs \(\rightarrow\) Biological Parameters \(\rightarrow\) Lactational Amenorrhea (LAM)
Overview
Breastfeeding can play an important role in improving maternal and child health by increasing birth intervals due to the temporary contraceptive effect from lactation. This method, called the lactational amenorrhea method (LAM), is defined in the 1988 Bellagio Consensus as the informed use of breastfeeding as a contraceptive by a woman who is still amenorrheic and who does not feed her baby with supplements for up to 6 months after delivery.[1] Correct use of LAM means adherence to the three LAM criteria of 1) no resumption of menses; 2) not supplementing regularly or allowing long periods without breastfeeding, day or night; and 3) baby not aged older than 6 months, with some monthly deviation allowed from the feeding criteria.[2] Incorrect LAM use is defined as continued reliance on LAM when any of these three criteria are no longer met.
Virtually all women, in a short period of time postpartum, will be amenorrheic, regardless of their breastfeeding status.[3] The high efficacy is due in part to the fact that most women, whether contracepting or not, will be anovulatory and cannot become pregnant in the first 6-12 weeks postpartum.[2,3] However, this protection declines with time, and the risk of return of menses and ovulation, and subsequent risk of pregnancy, differs based on breastfeeding status. Breastfeeding women have longer durations of amenorrhea than non-breastfeeders, and breastfeeding women who delay supplementation and/or nurse more frequently have the longest duration of amenorrhea. Among those breastfeeding, women who are fully breastfeeding have ovulation delayed longer than women who have begun supplementing.[4]
Several studies show that up to 50% of women ovulated before resumption of menses,[4] so women could be experiencing amenorrhea. yet still be at risk for pregnancy, though this risk is small. Once menstruation has returned, breastfeeding can no longer be relied upon to protect the nursing mother against pregnancy, as mothers who are menstruating during breastfeeding have a chance of contraception that is less than normally cycling non-lactating women, but high enough to require alternative forms of contraception.[5,6,7]
The impact of the timing of supplemental feeding on the efficacy of lactational amenorrhea and return of menses for the mother is debated. Two studies suggest that LAM can be relied upon as the sole method of highly effective contraception up to six months, irrespective of when supplements are introduced to the infant’s diet.[5,8] However, while partial breastfeeding still suppresses fertility, supplementation reduces the child’s need to suckle, which decreases breast stimulus and quickens menstruation.[8] Although supplementation with other foods decreases protective effects of breastfeeding against pregnancy, women who continue to breastfeed beyond 6 months may still experience subfertility, albeit at a rate of pregnancy higher than that experienced at 6 months.[9] Two studies find that after 9 months postpartum, there is no protective effect of breastfeeding.[6,10]
Data
LAM is highly effective against ovulation and pregnancy, with the maximum benefit for spacing and greatest protection against ovulation and pregnancy amongst women who are exclusively or fully breastfeeding.[4,8,11] Several studies find that with correct use among amenorrheic women who are exclusively or fully breastfeeding, efficacy rates of LAM as a contraceptive method are 98%. A Cochrane review conducted by Van der Wijden et al. (2015)[11] reported life table pregnancy rates of LAM users ranging from 0.45%-2.45% at 6 months. LAM is equally effective in a variety of healthcare settings, both in developed and developing countries.[2] Kennedy (1992)[8] found cumulative pregnancy rates of 2.9 and 5.9 per 100 women at 6 and 12 months, respectively, compared with 0.7 among LAM users at 6 months. Other estimates find that the efficacy for correct use of LAM is 98.5% at 6 months and 92.2% at 12 months.[2] Another study in India of 5,161 households found that among women who were breastfeeding compared to not breastfeeding, the relative risk of return to menses at time \(t\) was 0.47 (SE: 0.15) for \(0<t<6\) months and 0.93 (SE: 0.36) for \(6<t<9\) months.[10]
| Study | 6-month efficacy | 9-month efficacy | 12-month efficacy |
|---|---|---|---|
| Bellagio consensus 1988[1] | More than 98% for fully or nearly fully breastfeeding | — | — |
| Labbok 1997[2] | 98.5% for correct use | — | — |
| 98.3% for incorrect use | — | 92.2% | |
| 98.0% for lactational amenorrhea | — | 91.2% | |
| Kennedy 1992[8] | 99.3% for ‘correct use’ | — | — |
| 97.1% for lactational amenorrhea | — | 94.1% | |
| 92.4% for only baby less than 6 mos | — | 82.8% | |
| Ramos 1996[12] | 99.0% for correct use | — | — |
| 97.5% for incorrect use | — | — | |
| 98.5% for all women during correct or incorrect use | — | — | |
| 99.1% for lactational amenorrhea | 97.4% | 97.4% | |
| Short 1991[5] | 98.3% | — | 93.0% |
| Van der Wijden 2015[11] | 97.55, 99.55% in two controlled studies of LAM | — | — |
| 92.5-100% in six uncontrolled studies of LAM | — | — | |
| 98.8-99.12% among fully breastfeeding women who were amenorrheic who were not aware of LAM as a contraceptive method | — | — |
Parameters
As a conservative assumption, we assume no protective efficacy of LAM after 9 months. Based on estimates from the literature, we assume a LAM efficacy for exclusive breastfeeding of around 98% up to 6 months post-partum (i.e. failure rate of 2%), and around 97% up to 9 months post-partum. For women who are non-exclusively breastfeeding we model a relative rate of pregnancy at 6 months and 9 months based on estimates from Dihidar 2002.[10]
When drawing parameters, we constrain the failure rate/relative rate for 0-6 months to be lower than for 6-9 months.
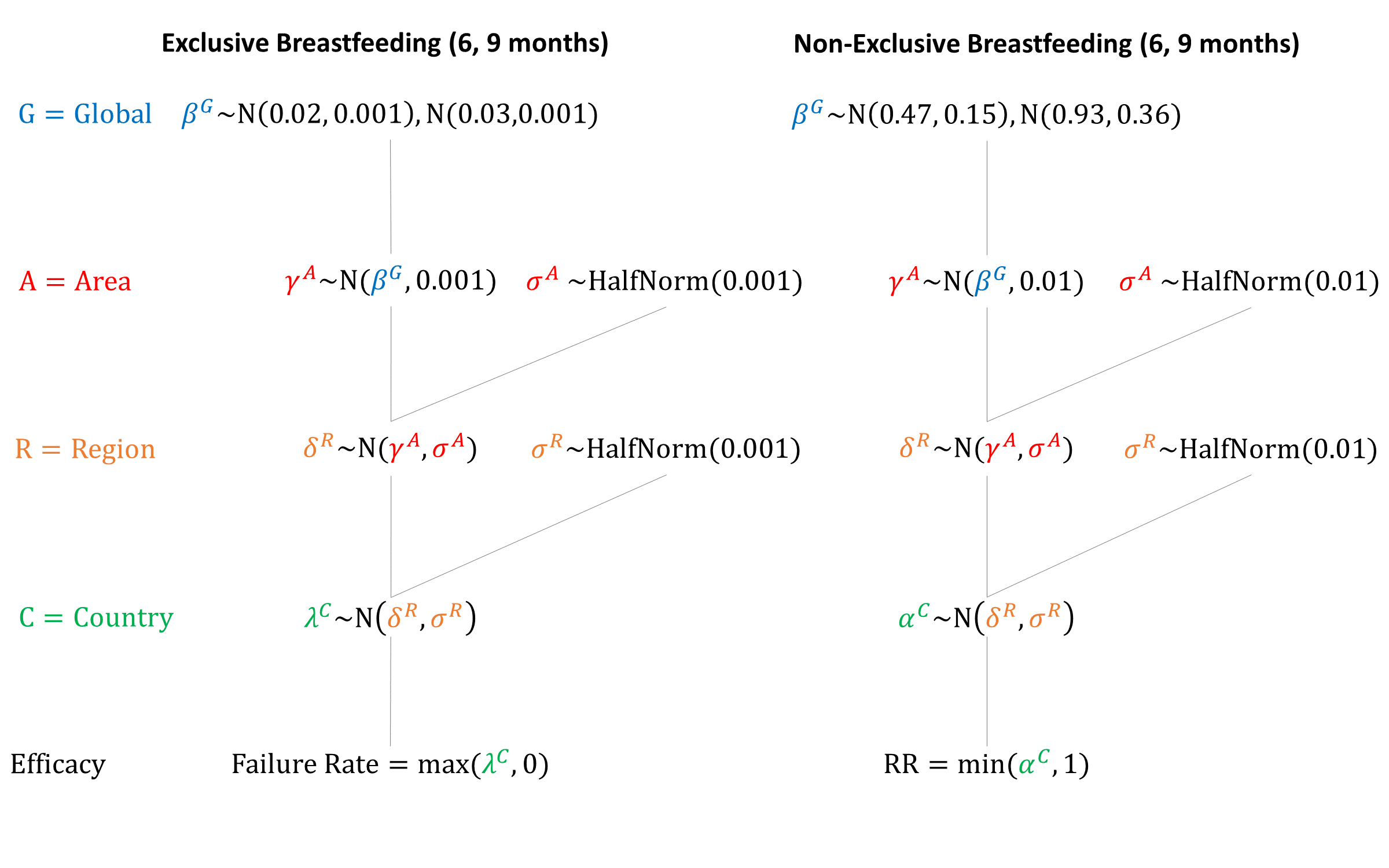
Priors
Model Implementation
At delivery, a woman’s breastfeeding status (exclusive/non-exclusive) and duration (months) are simulated (see Breastfeeding). If the woman breastfeeds exclusively, the failure rate of LAM is used, converted to monthly probabilities assuming a constant failure rate over the relevant period (6 months or 9 months). If a woman breastfeeds non-exclusively, the associated relative rate of pregnancy is applied to the age-specific pregnancy rate. We assume that the efficacy of LAM and contraceptive methods are independent.
References
- Kennedy KI, Rivera R, McNeilly AS. Consensus statement on the use of breastfeeding as a family planning method. Contraception 1989; 39(5): 477-96. DOI: https://doi.org/10.1016/0010-7824(89)90103-0
- Labbok MH, Hight-Laukaran V, Peterson AE, Fletcher V, von Hertzen H, Van Look PF. Multicenter study of the Lactational Amenorrhea Method (LAM): I. Efficacy, duration, and implications for clinical application. Contraception 1997; 55(6): 327-336. DOI: https://doi.org/10.1016/s0010-7824(97)00040-1
- Bracher M. Breastfeeding, lactational infecundity, contraception and the spacing of births: implications of the Bellagio Consensus Statement. Health Transit Rev 1992; 2(1): 19-47. PMID: https://www.ncbi.nlm.nih.gov/pubmed/10148664
- Bender DE, Dusch E, McCann MF. From efficacy to effectiveness: selecting indicators for a community-based lactational amenorrhea method promotion programme. J Biosoc Sci 1998; 30(2): 193-225. DOI: https://doi.org/10.1017/s002193209800193x
- Short RV, Lewis PR, Renfree MB, Shaw G. Contraceptive effects of extended lactational amenorrhoea: beyond the Bellagio Consensus. Lancet 1991; 337: 715-7. DOI: https://doi.org/10.1016/0140-6736(91)90288-z
- Howie PW. Natural regulation of fertility. Br Med Bull 1993; 49(1): 182-199. DOI: https://doi.org/10.1093/oxfordjournals.bmb.a072597
- Trussell J. Contraceptive efficacy. In Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, Kowal D. Contraceptive Technology: Nineteenth Revised Edition. New York NY: Ardent Media, 2007. http://www.contraceptivetechnology.org/wp-content/uploads/2013/09/Contraceptive-Failure-Rates.pdf
- Kennedy KI, Visness CM. Contraceptive efficacy of lactational amenorrhoea. Lancet 1992; 339: 227-30. DOI: https://doi.org/10.1016/0140-6736(92)90018-x
- Kennedy KI, Labbok MH, Van Look PF. Lactational amenorrhea method for family planning. Int J Gynaecol Obstet 1996; 54(1): 55-57. DOI: https://doi.org/10.1016/0020-7292(96)02670-7
- Dihidar S, Bhattacharya BN, Mukherjee KL. Description of breastfeeding practices among poorer sections in Calcutta Metropolitan Area and its impact on postpartum infecundity. J Child Health Care 2002; 6(3): 203-19. DOI: https://doi.org/10.1177/136749350200600301
- Van der Wijden C, Manion C. Lactational amenorrhoea method for family planning. Cochrane Database Syst Rev 2015; CD001329. DOI: https://doi.org/10.1002/14651858.CD001329.pub2
- Ramos R, Kennedy KI, Visness CM. Effectiveness of lactational amenorrhoea in prevention of pregnancy in Manila, the Philippines: non-comparative prospective trial. BMJ 1996; 313: 909-12. DOI: https://doi.org/10.1136/bmj.313.7062.909
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu