Active Management of Labor
Model Inputs \(\rightarrow\) Clinical Interventions \(\rightarrow\) Active Management of Labor
Overview
After delivery of the baby, continued uterine contractions normally facilitate the shrinking of the uterus, separation of the placenta, and closing maternal blood vessels within the uterine wall. The purpose of management of the third stage of labor is to ensure that this happens, thus enabling the prevention/early detection of uterine atony, the most common cause of PPH.[1] Labor management involves either a “hands-off” approach (Expectant management) or a “hands-on” approach (Active management).
Expectant management (also called physiological or conservative management of labor) involves watching out for signs of placental separation and allowing the placenta to deliver spontaneously, or via the aid of gravity or nipple stimulation. On the other hand, active management involves interventions that facilitate the third stage of labor.
Active management of the third stage involves three components: 1) giving a drug (a uterotonic) to contract the uterus; 2) clamping the cord early (usually before, alongside, or immediately after giving the uterotonic), and this is before cord pulsation stops; 3) traction is applied to the cord with counter-pressure on the uterus to deliver the placenta (controlled cord traction). Specific ways the three components are used often vary. Mixed management uses some, but not all, of the three components.[2]
Data
While active management is commonly used for facility births, it is not necessarily universally practiced. A survey of members of the Royal College of Obstetricians and Gynaecologists (RCOG) and members of the Royal College of Midwives (RCM) in the UK found that the majority (94% and 71%, respectively) ‘always’ or ‘usually’ use active management, and 73% and 40% clamp the cord within 20 seconds.[3]
A recent Cochrane review reported the effect of active management compared to expectant management. For severe PPH (1000ml+), they reported a risk ratio of 0.34 (95% CI 0.14-0.87) - however, the authors stated that they were uncertain of this finding because of the very low-quality evidence.[2] Another Cochrane review compared prophylactic oxytocin (a critical component of active management) with placebo, and found that it reduced the risk of PPH (>500mL), with a risk ratio of 0.51 (95% CI 0.37-0.72), and reduced blood loss of >1000mL with a risk ratio of 0.59 (95% CI 0.42-0.83).[4] A systematic review of active management vs expectant management found that it reduced overall PPH incidence by 26% (17.96% [95% CI 16.97-18.95] vs 13.22% [95% CI 12.87-13.57]), and severe PPH by 22% (3.84% [95% CI 3.31-4.37] vs 2.99% [95% CI 2.80-3.18]).[5]
We could not find estimates of the effect of expectant management of labor compared to no management. It is also difficult to determine where expectant management is being practiced - given its low-tech approach, it may be common practice for mothers at home to use gravity/nipple stimulation. As a conservative assumption we do not explicitly model expectant management, but rather assume it is a tacit component of all natural history deliveries. Given that our estimates of the efficacy of active management are compared to expectant management, this is also necessary so that we do not bias our modeled effects of active management.
Parameters
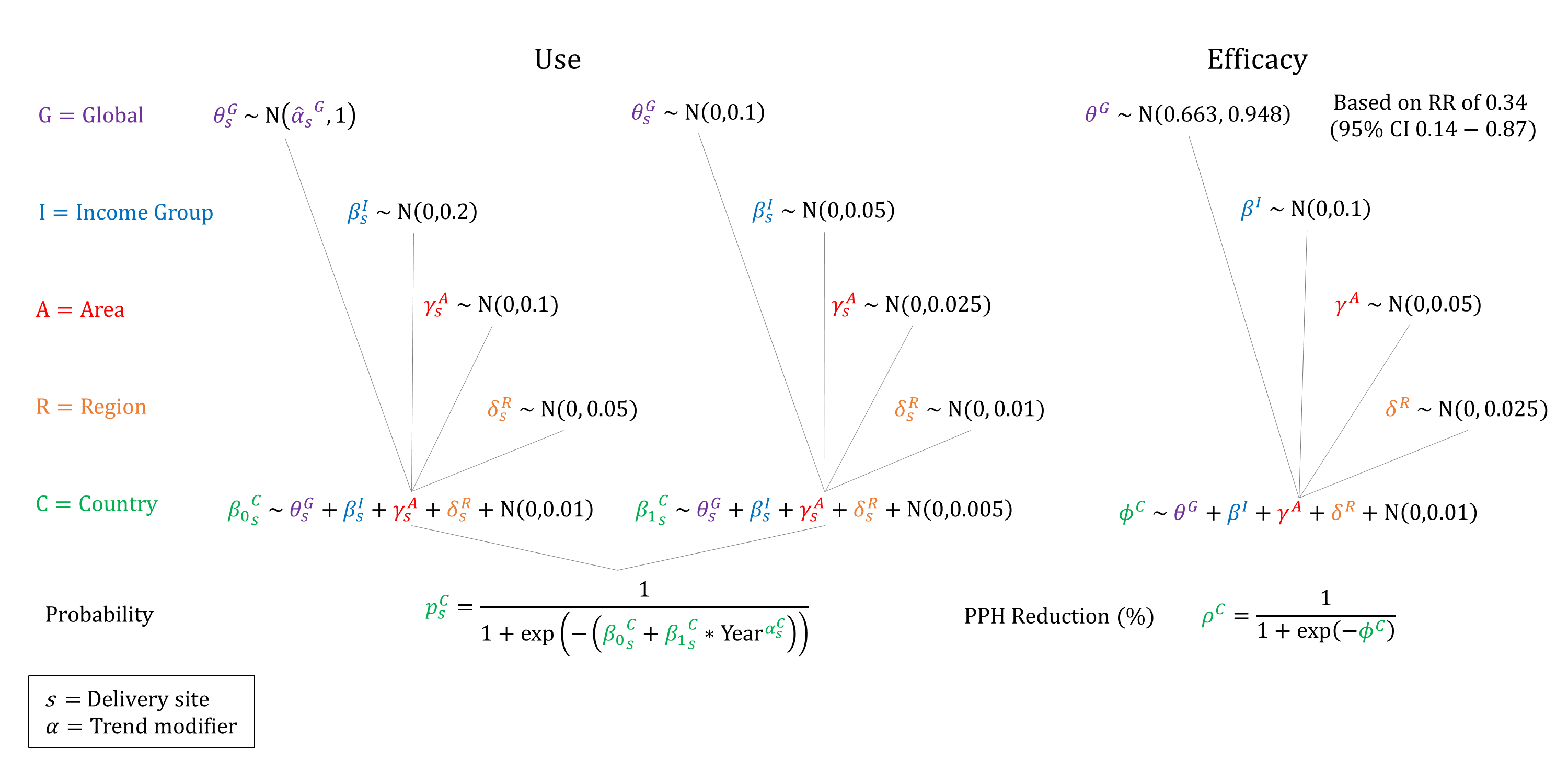
We model the use and efficacy of active management. We assume that the use of active management increases by delivery site and income group, and that it is not available at home. We assume that use of active management increases over time and so constrain the year coefficient to be non-negative when sampling. We assume that the efficacy of active management on reducing PPH incidence is non-differential by severity.
Priors
Model Implementation
Conditional on the site of delivery we simulate the probability that active management will be used and its efficacy on reducing PPH incidence.
References
- World Health Organization. WHO guidelines for the management of postpartum haemorrhage and retained placenta, 2009. Available: http://apps.who.int/iris/bitstream/10665/44171/1/9789241598514_eng.pdf.
- Begley CM, Gyte GM, Devane D, McGuire W, Weeks A, Biesty LM. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev 2019; 2(2): CD007412. DOI: https://doi.org/10.1002/14651858.cd007412.pub5
- Farrar D, Tuffnell D, Airey R, Duley L. Care during the third stage of labour: a postal survey of UK midwives and obstetricians. BMC Pregnancy Childbirth 2010; 10: 23. DOI: https://doi.org/10.1186/1471-2393-10-23
- Salati JA, Leathersich SJ, Williams MJ, Cuthbert A, Tolosa JE. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database Syst Rev 2019; 4(4): CD001808. DOI: https://doi.org/10.1002/14651858.cd001808.pub3
- Carroli G, Cuesta C, Abalos E, Gulmezoglu AM. Epidemiology of postpartum haemorrhage: a systematic review. Best Pract Res Clin Obstet Gynaecol 2008; 22(6): 999-1012. DOI: https://doi.org/10.1016/j.bpobgyn.2008.08.004
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu