Sepsis
Model Inputs \(\rightarrow\) Obstetric Complications \(\rightarrow\) Sepsis
Overview
Puerperal (or postpartum) infection is generally defined as any bacterial infection of the female reproductive tract following childbirth or miscarriage. Signs and symptoms usually include a fever greater than 38.0°C (100.4°F), chills, lower abdominal pain, and possibly bad-smelling vaginal discharge.[1] Puerperal sepsis is the pregnancy-related infection that causes the greatest concern because of its severity. While various definitions of sepsis have been used in the literature,[2] the WHO convened a group of experts to propose an up-to-date global definition for maternal sepsis, defined as “a life-threatening condition defined as organ dysfunction resulting from infection during pregnancy, childbirth, post-abortion, or postpartum period”.[3]
Data
Incidence
In the eighteenth and nineteenth centuries it is estimated that there were roughly 6-9 cases of sepsis per 1,000 deliveries in Europe, with far more occurring during epidemics of ‘puerperal fever’.[4] With modern birth practices, available data on pregnancy-related sepsis from high income countries report incidences ranging from 9 to 49 per 100,000 deliveries.[5] Scarce data from low income countries makes the incidence of sepsis difficult to determine.[6] According to Filippi (2016),[7] there has been no recent published review of sepsis incidence since the work conducted for the 2000 Global Burden of Disease.[8] That review calculated that the incidence of sepsis ranged from 2.7 and 5.2 per 100 live births according to world region. Since then, a recent community-based study in India found that the incidence of puerperal sepsis in the first week postpartum was 1.2 percent after home delivery and 1.4 percent after facility-based delivery.[9] The incidence of fever was higher at 4 percent overall in the same Indian study.[9] Another study in India found a high incidence of puerperal infections at home (10 percent) and of fever (12 percent), but the study used broader definitions and followed women for 28 days.[10] Another study in Pakistan found that out of 3,316 obstetrical admissions, 3.89% had puerperal sepsis.[11]
There is a growing body of evidence that the single most important risk factor for postpartum infection is caesarean section.[12] Women who undergo caesarean section have a five to 20-fold greater risk for infection (and infectious morbidity) compared with a vaginal birth.[13] A study from Denmark found that within 30 days after birth, 1.6% of women who delivered vaginally acquired an infection, compared to 7.6% of women who had a caesarean section - an almost five-fold increase in the risk of infection.[14] Women undergoing cesarean section can be divided into low- and high-risk groups for infection, with women undergoing an elective procedure at lowest risk, while women at high risk include those undergoing cesarean section after rupture of the membranes or onset of labor.[15] A previous Cochrane systematic review on antibiotic prophylaxis for caesarean section found an average rate of endometritis in women undergoing caesarean section without antibiotic coverage of 9.2% for elective caesarean sections and 28.6% for non-elective caesarean sections, while the use of antibiotic prophylaxis reduced the incidence of endometritis by two-thirds to three-quarters for all studies combined.[16] Antibiotic prophylaxis thus mitigates the risk of infection, but it is nevertheless higher after a caesarean section than after a spontaneous vaginal delivery.[12]
Morbidity/Mortality
In historical epidemics of puerperal fever in Europe, the case fatality rate tended to be highest at the beginning of the epidemic, sometimes reaching levels of 70%-80% before declining over a period of a couple of years, while it is estimated that case fatality rates in sporadic cases were likely in the region of 25%-30% before the introduction of sulphonamides in the mid-1930s.[4] In modern times, mortality from maternal sepsis in high income countries is estimated to be around 17 deaths per 100,000 live births, but it may be increasing.[6,17,18] Previous studies from low and middle income countries report case fatality rates between 4% and 50%.[2,8] A review conducted by the Disease Control Priorities Project (DCP2)[19] reported an average CFR of 1.3%, while some studies reported higher rates: 4.1%[20] and 8.5%.[11] Determining risk factors for maternal sepsis mortality is difficult as few deaths occur in countries where there are resources to accurately measure risk, rendering studies insufficiently powered to draw conclusions.[21] However, we do assume increased risk of death for women with anemia.[22]
Apart from death, women who experience peripartum infections are also prone to long-term disabilities such as chronic pelvic pain, fallopian tube blockage, and secondary infertility.[23] Estimates of the risk of infertility given sepsis are scarce however. The GBD 2000 assumed that puerperal infection resulted in infertility between 5% in developed countries to 12% in developing countries.[24]
Parameters
We model two levels of sepsis severity: Moderate and Severe. We constrain incidence to decrease by severity, and risk of morbidity/mortality to increase by severity when sampling parameters.
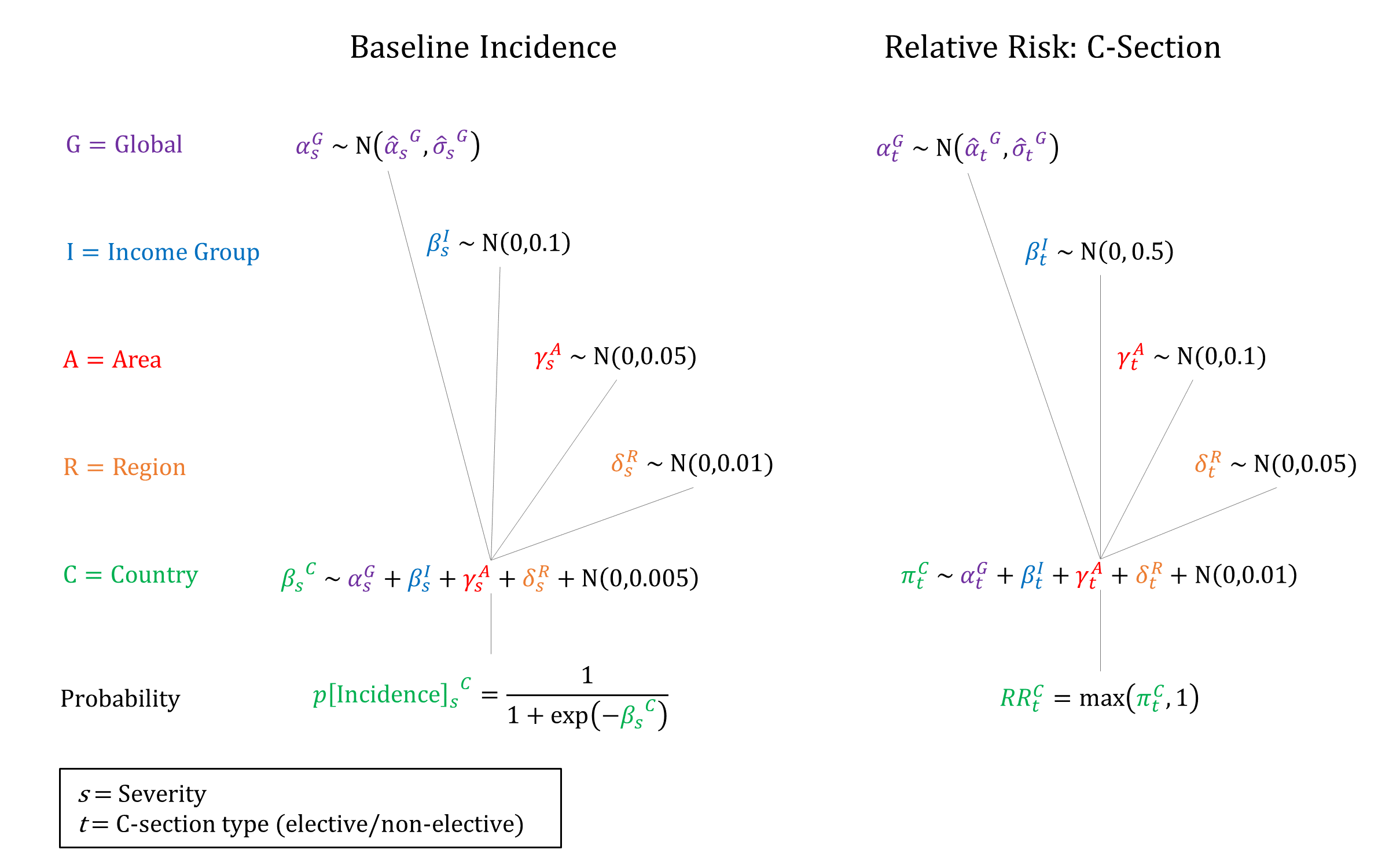
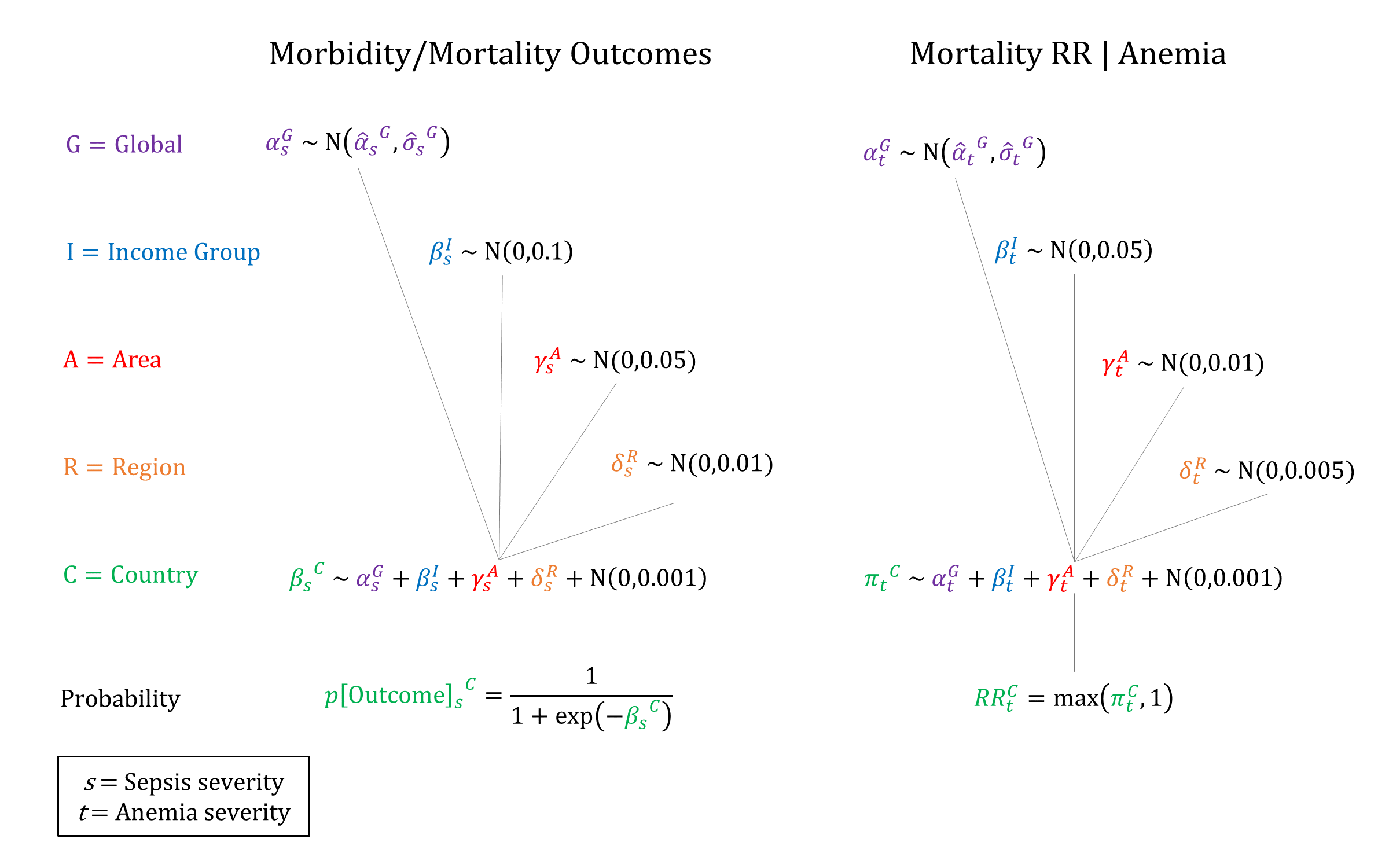
Priors
Model Implementation
At the time of delivery, the incidence and outcomes of Sepsis are simulated, together with the availability and efficacy of interventions that modify the ‘natural history’ probabilities.
References
- Cunningham FG, Leveno KJ, Bloom SL et al. Chapter 37: Puerperal Complications. In: Williams Obstetrics (24th ed). McGraw-Hill Medical, New York, NY, 2014. Available at: https://accessmedicine.mhmedical.com/content.aspx?bookid=1918§ionid=141464707
- Bonet M, Souza JP, Abalos E, et al. The global maternal sepsis study and awareness campaign (GLOSS): study protocol. Reprod Health 2018; 15(1): 16. DOI: https://doi.org/10.1186/s12978-017-0437-8
- World Health Organization. Statement on Maternal Sepsis. 2017. Available at: http://apps.who.int/iris/bitstream/10665/254608/1/WHO-RHR-17.02-eng.pdf?ua=1
- Loudon I. The Tragedy of Childbed Fever. Oxford University Press, 2000. DOI: https://doi.org/10.1093/acprof:oso/9780198204992.001.0001
- Oud L. Pregnancy-associated severe sepsis: contemporary state and future challenges. Infect Dis Ther 2014; 3(2): 175–89. DOI: https://doi.org/10.1007/s40121-014-0037-7
- van Dillen J, Zwart J, Schutte J, van Roosmalen J. Maternal sepsis: epidemiology, etiology and outcome. Curr Opin Infect Dis 2010; 23(3): 249-54. DOI: https://doi.org/10.1097/qco.0b013e328339257c
- Filippi V, Chou D, Ronsmans C, Graham W, Say L. Chapter 3. Levels and causes of maternal mortality and morbidity. In: Black RE, Laxminarayan L, Walker N, Temmerman M, eds. Disease control priorities 3rd edn. Volume 2. Reproductive, maternal, newborn and child health. Washington, DC: World Bank, 2016. Available at: https://www.ncbi.nlm.nih.gov/books/NBK361917/
- Dolea C, Stein C. Global Burden of Maternal Sepsis in the Year 2000. Evidence and information for policy (EIP). Global Burden of Disease Working Paper, 2003. Available at http://www.who.int/healthinfo/statistics/bod_maternalsepsis.pdf.
- Iyengar K. Early postpartum maternal morbidity among rural women of Rajasthan, India: a community-based study. J Health Popul Nutr 2012; 30(2): 213-25. DOI: https://doi.org/10.3329/jhpn.v30i2.11316
- Bang RA, Bang AT, Reddy MH, Deshmukh MD, Baitule SB, Filippi V. Maternal morbidity during labour and the puerperium in rural homes and the need for medical attention: A prospective observational study in Gadchiroli, India. BJOG 2004; 111(3): 231-8. DOI: https://doi.org/10.1111/j.1471-0528.2004.00063.x
- Khaskheli MN, Baloch S, Sheeba A. Risk factors and complications of puerperal sepsis at a tertiary healthcare centre. Pak J Med Sci 2013; 29(4): 972-6. DOI: https://doi.org/10.12669/pjms.294.3389
- Buddeberg BS, Aveling W. Puerperal sepsis in the 21st century: progress, new challenges and the situation worldwide. Postgrad Med J 2015; 91(1080): 572-8. DOI: https://doi.org/10.1136/postgradmedj-2015-133475
- Smaill FM, Grivell RM. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database Syst Rev 2014; 10: CD007482. DOI: https://doi.org/10.1002/14651858.CD007482.pub3
- Leth RA, Møller JK, Thomsen RW, Uldbjerg M, Nørgaard M. Risk of selected postpartum infections after cesarean section compared with vaginal birth: a five-year cohort study of 32,468 women. Acta Obstet Gynecol Scand 2009; 88(9): 976–83. DOI: https://doi.org/10.1080/00016340903147405
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol 2011; 117(6): 1472-83. DOI: https://doi.org/10.1097/aog.0b013e3182238c31
- Smaill F, Hofmyer GJ. Antibiotic prophylaxis for caesarean section. Cochrane Database Syst Rev 2002; 3: CD000933. DOI: https://doi.org/10.1002/14651858.cd000933
- Bauer ME, Bateman BT, Bauer ST, Shanks AM, Mhyre JM. Maternal sepsis mortality and morbidity during hospitalization for delivery: temporal trends and independent associations for severe sepsis. Anesth Analg 2013; 117(4): 944–50. DOI: https://doi.org/10.1213/ane.0b013e3182a009c3
- Vaught AJ. Maternal sepsis. Semin Perinatol 2018; 42(1): 9-12. DOI: https://doi.org/10.1053/j.semperi.2017.11.003
- Graham WJ, Cairns J, Bhattacharya S, et al. Maternal and Perinatal Conditions. In: Jamison DT, Breman JG, Measham AR, et al, eds. Disease Control Priorities in Developing Countries. 2nd edition. Washington (DC): World Bank; 2006. Available at: https://www.ncbi.nlm.nih.gov/books/NBK11742/
- Dare FO, Bako AU, Ezechi OC. Puerperal sepsis: a preventable post-partum complication. Trop Doct 1998; 28(2): 92-5. DOI: https://doi.org/10.1177/004947559802800212
- Acosta CD, Knight M. Sepsis and maternal mortality. Curr Opin Obstet Gynecol 2013; 25(2): 109-16. DOI: https://doi.org/10.1097/gco.0b013e32835e0e82
- Brabin BJ, Hakimi M, Pelletier D. An analysis of anemia and pregnancy-related maternal mortality. J Nutr 2001; 131(2S-2): 604S-614S. DOI: https://doi.org/10.1093/jn/131.2.604s
- World Health Organization. WHO recommendations for prevention and treatment of maternal peripartum infections. 2015. Available at: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/peripartum-infections-guidelines/en/
- Abouzahr C, Aaahman E, Guidotti R. Puerperal sepsis and other puerperal infections. In Health dimensions of sex and reproduction: the global burden of sexually transmitted diseases, maternal conditions, perinatal disorders, and congenital anomalies, eds. CJL Murray and AD Lopez, WHO 1998. https://apps.who.int/iris/handle/10665/42161
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu