Clean Delivery
Model Inputs \(\rightarrow\) Clinical Interventions \(\rightarrow\) Clean Delivery
Overview
The most effective interventions for preventing maternal sepsis are the use of antiseptics and observation of stringent infection control measures to limit the spread of microorganisms, especially within hospital environments. General measures such as handwashing with soap are widely accepted practices to prevent infection transmission.[1]
Clean birth kits (CBKs) for home use have also been developed to prevent infection, which the WHO recommends contain at a minimum: soap, plastic sheet, razor blade, cord ties, alcohol swabs, and gauze.[2,3]
Data
A systematic review of CBK use found that reported usage varied widely, with estimates between 8% and 99% for Nepal alone, depending on the study.[3] Proper use of the items in the CBK also varied substantially.[3] For facility births, an assessment of a sample of facilities in Gujarat in 2009 found that 70% of respondents said that standard infection control procedures were followed, but a written procedure was only available in 5% of facilities.[4] Furthermore, the study found that alcohol rubs were not used for hand cleaning, and surgical gloves were reused in over 70% of facilities, especially for vaginal examinations in the labor room.
Although there are no systematic reviews evaluating the effect of handwashing on maternal mortality from sepsis, the work of Semmelweis in the mid-19th century shed light on the epidemiological basis of puerperal sepsis and confirmed the impact of this simple and inexpensive measure on reducing maternal and morbidity.[1,5]
A 2012 systematic review concluded that while providing birth kits to facilitate clean practices seems common sense, there is no evidence to indicate effects (positive or negative) independent of those achieved by a broader intervention package.[2] A 2015 Cochrane review examined community intervention packages, in which a large component was increasing use of clean delivery kits: uptake increased by 82% while maternal mortality decreased (RR 0.80, [95% CI 0.64-1.00]), and maternal morbidity decreased (RR 0.75, [95% CI 0.61-0.92]).[6] However, since many things were changed (including a 20% increase in facility deliveries), and the deaths were not broken out by cause, it is difficult to ascertain what effect (if any) any single component, such as clean delivery kits, had on any particular delivery complication. A 2020 systematic review also found that the evaluation of CBKs was rarely found in isolation from intervention packages involving education programmes or service delivery, and that the components of the kits varied in each study, limiting the comparability of the studies.[3] While the studies could not be pooled because of heterogeneity, they did find reductions in sepsis.
A cluster randomised controlled trial from Pakistan reported a reduction in puerperal sepsis (OR 0.18, 95% CI 0.14-0.22) with the introduction of community-based intervention packages including provision of CBKs.[7] A cross-sectional study from Egypt reported that mothers who used a CBK were less likely to develop puerperal sepsis (OR 0.11, 95% CI 0.01-1.06).[8] Two studies in Tanzania by Mosha (2005)[9] and Winani (2007)[10] concluded that women who bathed before delivery and women who used a clean delivery kit were 2.6 and 3.2 times less likely to develop puerperal sepsis than women who did not, respectively. A case control study from Ethiopia found that women who were given a CBK had fewer symptoms of puerperal sepsis (p<0.00).[11]
We set wide priors for availability of clean delivery, and set priors for the efficacy on reduction of sepsis centered around 95%. Note that this parameter governs the maximum possible full efficacy - the actual modelled effect is modified by site-specific quality of care parameters for each country.
Parameters
We model the use and efficacy of clean delivery practices, and assume that use increases by delivery site and income group. We assume that clean delivery practices increase over time and so constrain the year coefficient to be non-negative when sampling. We assume that the efficacy of clean delivery on reducing sepsis incidence is non-differential by severity.
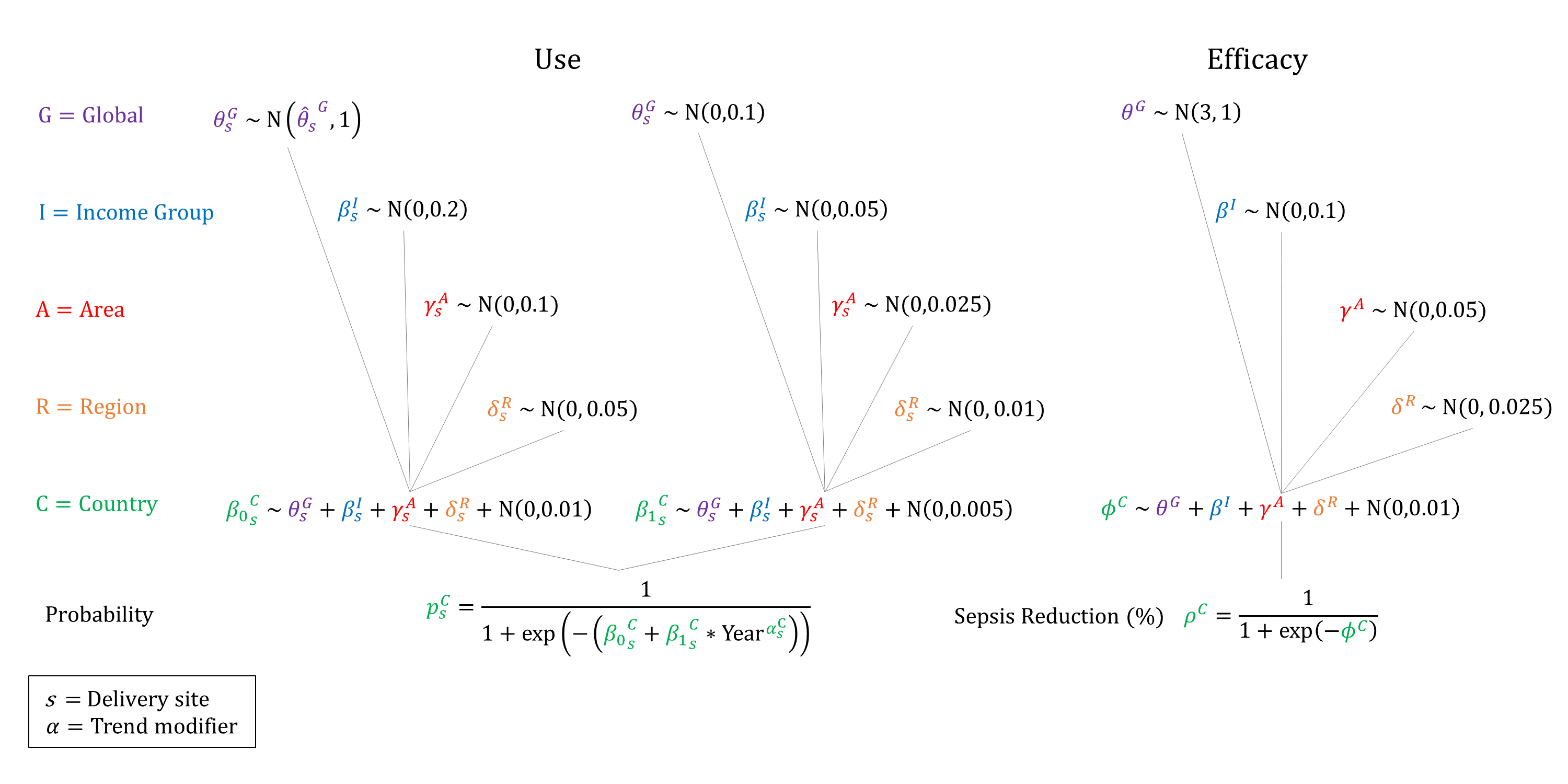
Priors
Model Implementation
Conditional on the site of delivery we simulate the probability that the delivery will be ‘clean’ and the impact on reducing the incidence of sepsis.
References
- Gülmezoglu, Lawrie TA, Hezelgrave N, et al. Chapter 7. Interventions to Reduce Maternal and Child Morbidity and Mortality. In: Black RE, Laxminarayan L, Walker N, eds. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016. DOI: https://doi.org/10.1596/978-1-4648-0348-2_ch7
- Hundley V, Avan B, Braunholtz D, Graham WJ. Are birth kits a good idea? A systematic review of the evidence. Midwifery 2012; 28(2): 204-215. DOI: https://doi.org/10.1016/j.midw.2011.03.004
- Lassi ZS, Fisher Z, Andraweera P, Cummins A, Roberts CT. Effectiveness of birthing kits for clean childbirth: a systematic review. Int Health 2020; 12(1): 3-10. DOI: https://doi.org/10.1093/inthealth/ihz022
- Mehta R, Mavalankar DV, Ramani KV, Sharma S, Hussein J. Infection control in delivery care units, Gujarat state, India: a needs assessment. BMC Pregnancy Childbirth 2011; 11: 37. DOI: https://doi.org/10.1186/1471-2393-11-37
- Noakes TD, Borresen J, Hew-Butler T, Lambert MI, Jordaan E. Semmelweis and the aetiology of puerperal sepsis 160 years on: an historical review. Epidemiol Infect 2008; 136(1): 1-9. DOI: https://doi.org/10.1017/s0950268807008746
- Lassi ZS, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev 2015; 3: CD007754. DOI: https://doi.org/10.1002/14651858.cd007754.pub3
- Jokhio AH, Winter HR, Cheng KK. An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med 2005; 352(20): 2091–9. DOI: https://doi.org/10.1056/nejmsa042830
- Darmstadt GL, Hassan M, Balsara ZP, Winch PJ, Gipson R, Santosham M. Impact of clean delivery-kit use on newborn umbilical cord and maternal puerperal infections in Egypt. J Health Popul Nutr 2009; 27(6): 746-54. DOI: https://doi.org/10.3329/jhpn.v27i6.4326
- Mosha F, Winani S, Wood S, Changalucha J, Ngasalla B. Evaluation of the effectiveness of a clean delivery kit intervention in preventing cord infection and puerperal sepsis among neonates and their mothers in rural Mwanza Region, Tanzania. Tanzan Health Res Bull 2005; 7(3): 185-8. DOI: https://doi.org/10.4314/thrb.v7i3.14258
- Winani S, Wood S, Coffey P, Chirwa T, Mosha F, Changalucha J. Use of a clean delivery kit and factors associated with cord infection and puerperal sepsis in Mwanza, Tanzania. J Midwifery Womens Health 2007; 52(1): 37-43. DOI: https://doi.org/10.1016/j.jmwh.2006.09.004
- Onolemhemhen D. The Ethiopian Birth Kit Project. Paper presented at: 13th World Conference on Public health 2012; Addis Abba, Ethiopia. Available at: https://www.researchgate.net/publication/268139777_The_Ethiopian_Birth_Kit_Project
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu