Stillbirths
Model Inputs \(\rightarrow\) Biological Parameters \(\rightarrow\) Stillbirths
Overview
The WHO recommends that stillbirth be defined as a baby born with no signs of life at or after 28 weeks’ gestation.[1] Other definitions are based on birthweight. However, it is argued that a gestational age threshold is more appropriate as it is a better predictor of maturity (and hence viability), with many fetuses at risk of stillbirth having preceding fetal growth restriction.[2,3] Intrapartum stillbirth is a death which occurs after the onset of labour but before birth.
Data
The estimated global stillbirth rate in 2015 was 18.4 per 1000 births, down from 24.7 in 2000, with an estimated 2.6 million stillbirths per year.[4] It is estimated that 98% of all stillbirths occur in low-income and middle-income countries, with 77% in south Asia and sub-Saharan Africa.[4] Stillbirth rates are estimated to range from 3.4 per 1000 births in developed regions to 28.7 in sub-Saharan Africa, with intrapartum stillbirths estimated to account for 50% of stillbirths globally, ranging from 10% in developed countries to 60% in Southern Asia.[3]
An analysis of 18 countries with reliable data found that congenital abnormalities accounted for a median of only 7.4% of stillbirths.[3] Thus, disorders associated with many stillbirths are potentially modifiable and often coexist, such as maternal infections, non-communicable diseases, and nutrition and lifestyle factors.[3]
Maternal age (older than 35 years, or younger than 16 years) is also associated with increased risk of stillbirth.[3] Andersen (2000)[5] presents rates of stillbirth by maternal age group from a population-based register linkage study in Denmark. After adjusting the denominator by subtracting all induced abortions from the number of pregnancies, the adjusted risk of stillbirth was calculated by age group, resulting in rates around 3-4 per 1,000. Due to the high quality of obstetric and neonatal care in Denmark, we assume that intrapartum stillbirths are rare in this population,[3] and use these estimates as priors for rates of antepartum stillbirth.
Other risk factors for stillbirth include infections during pregnancy, such as malaria and syphilis.[3] Non-communicable diseases, especially hypertension and diabetes also have an impact, with about 10% of stillbirths globally attributed to these disorders.[3] Pregnancy lasting longer than 42 weeks is associated with increased risk, accounting for an estimated 14% of stillbirths worldwide.[3] We do not model these risk factors explicitly, but by using a hierarchical modeling approach we can implicitly account for these country-specific factors.
A systematic review of over 30 million birth outcomes found that male babies are at a higher risk of stillbirth, with a relative risk of 1.10 (95% CI: 1.07-1.13).[6] Probable explanations include X-linked congenital conditions, increased risk of preterm labour, and poor fetal growth for male babies.[3]
For intrapartum stillbirths, we model the risk related to obstructed labor and pre-eclampsia/eclampsia. For example, a review of studies found that prolonged deliveries which caused obstetric fistula also resulted in stillbirth for 78% to 96% of patients.[7] Another systematic review found the reported frequency of stillbirth associated with obstetric fistula ranged from 32.3% to 100%, with estimates from the largest studies around 92%.[8] Pre-eclampsia and eclampsia may contribute to poor fetal growth and have an estimated population attributable risk for stillbirths of about 5%.[3] As maternal age may be associated with these pregnancy complications, these increased risks may explain some of the association between maternal age and stillbirths.
In summary, we model the risk of stillbirth from 3 general causes:
| Stillbirth Type | Modeled Cause |
|---|---|
| Antepartum | Hierarchical spline model accounts for congenital risk, maternal age, and other country-specific risk factors such as infections and NCDs |
| Relative risk for male fetuses | |
| Intrapartum | Prolonged/obstructed labour |
| Antepartum/Intrapartum | Pre-eclampsia/eclampsia |
We include country-specific estimates of stillbirths as calibration targets.
Parameters
We fit quadratic B-splines to the midpoints of maternal age groups, based on stillbirth data from Andersen 2000.[5] Using a hierarchical model allows us to adjust these estimates to account for other country-specific risk factors.
Spline Width: 40
| Spline # | Knot Location | Height |
|---|---|---|
| 1 | 8 | \(N(6,0.75)\) |
| 2 | 22 \(^1/_3\) | \(N(4,0.1)\) |
| 3 | 37 \(^1/_3\) | \(N(4.5,0.3)\) |
| 4 | 52 | \(N(3.8,2)\) |
We extended the probability from age 50 to older ages.
We model a relative risk for males based on the estimated relative risk from Mondal 2014: RR = 1.10 (95% CI: 1.07-1.13).[6]
We used hierarchical models to account for risk of stillbirths from OL and HTN ([TO DO]see delivery complications…) We assume no excess risk for males from these intrapartum causes.
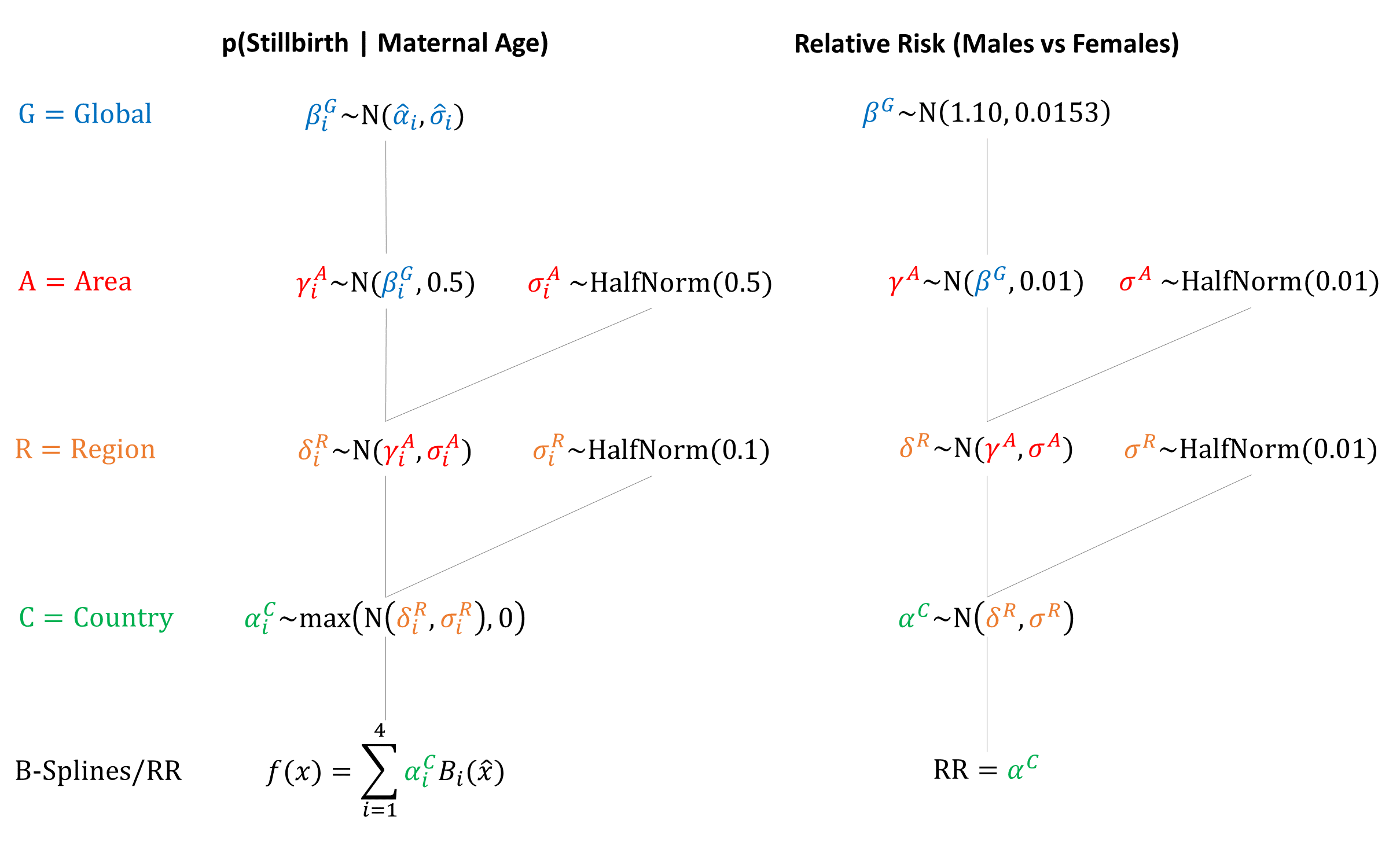
Priors
Model Implementation
Antepartum stillbirths are simulated based on country-specific risks modified by maternal age and fetus sex. Intrapartum stillbirths are simulated as a result of delivery complications (i.e. prolonged labour and pre-eclampsia/eclampsia). We assume that the risks of other delivery complications (i.e. post-partum hemorrhage and sepsis) are the same for both stillbirths and live births.
References
- World Health Organization. Stillbirths. https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/
- Mohangoo AD, Blondel B, Gissler M, Velebil P, Macfarlane A, Zeitlin J. International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age? PLoS One 2013; 8: e64869. DOI: https://doi.org/10.1371/journal.pone.0064869
- Lawn JE, Blencowe H, Wasiwa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 2016; 387(10018): 587-603. DOI: https://doi.org/10.1016/S0140-6736(15)00837-5
- Blencowe H, Cousens S, Jassir FB, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health 2016; 4(2): e98-e108. DOI: https://doi.org/10.1016/S2214-109X(15)00275-2
- Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ 2000; 320(7251): 1708-12. DOI: https://doi.org/10.1136/bmj.320.7251.1708
- Mondal D, Galloway TS, Bailey TC, Mathews F. Elevated risk of stillbirth in males: systematic review and meta-analysis of more than 30 million births. BMC Med 2014; 12: 220. DOI: https://doi.org/10.1186/s12916-014-0220-4
- Tebeu PM, Fomulu JN, Khaddaj S, de Bernis L, Delvaux T, Rochat CH. Risk factors for obstetric fistula: a clinical review. Int Urogynecol J 2012; 23: 387–94. DOI: https://doi.org/10.1007/s00192-011-1622-x
- Cowgill KD, Bishop J, Norgaard AK, Rubens C, Gravett MG. Obstetric fistula in low-resource countries: an under-valued and under-studied problem–systematic review of its incidence, prevalence, and association with stillbirth. BMC Pregnancy Childbirth 2015; 15: 193. DOI: https://doi.org/10.1186/s12884-015-0592-2
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu