Maternal Death Underreporting
Model Inputs \(\rightarrow\) Health System Parameters \(\rightarrow\) Maternal Death Underreporting
Overview
Empirical estimates of maternal mortality notoriously suffer from underreporting due to misclassification or omission altogether of maternal deaths. Civil registration vital statistics (CRVS) and health information systems in most developing countries are weak, and even estimates derived from complete CRVS systems in high income countries suffer from misclassification and underreporting of maternal deaths.[1] However, the amount of underestimation varies by setting and may change over time.
The accuracy of CRVS systems can be assessed by comparing the recorded mortality rates to those obtained from specialized studies which are rigorous assessments of maternal mortality. Previous work comparing study-based mortality to CRVS-based mortality found that study-based estimates of maternal mortality were around 150% higher than CRVS-based estimates, suggesting that CRVS systems do not adequately capture all maternal deaths.[2] Based on comparisons of maternal mortality between CRVS and specialized studies, the United Nations Maternal Mortality Estimation Inter-agency Group adjusts CRVS-based maternal mortality data in countries where specialized studies are available using the setting-specific adjustment factors, and adjusts all other countries using a global adjustment factor of 1.5.[3] An update to the UN approach found that the sensitivity of CRVS data for maternal deaths is poor, at 0.586 (80% CI 0.511-0.656), while specificity is good (0.9993, 80% CI 0.9990-0.9996).[4] The Global Burden of Disease also address underreporting of maternal mortality, and found that the net effect of data processing steps on vital registration data to correct for underreporting increased maternal deaths by 168%.[5]
However, underreporting is likely even higher in lower income settings with weaker or non-existent CRVS systems. Furthermore, adjusting the reported estimates of maternal mortality directly is a crude approach which does not account for the uncertainty around levels of underreporting, and is inconsistent with a fundamental tenet of Bayesian analysis: that data are fixed and parameters are random variables. We therefore include underreporting of maternal deaths as part of our modeled data generating process which gives rise to the empirical (though biased) maternal mortality estimates used to fit the model. This approach allows us to correct for underreporting in a Bayesian framework while also accounting for the (often substantial) uncertainty around levels and trends in underreporting of maternal deaths. To account for differential levels of maternal death underreporting in data from CRVS systems (based on passive reporting) and surveys (based on active case finding), we model two levels of underreporting (CRVS vs survey), and assume that survey-based estimates of maternal deaths are more complete than CRVS-based data. This is consistent with empirical data as surveys are often used to estimate the magnitude of underreporting present in CRVS data.
Data
We undertook a literature review to obtain estimates of maternal mortality underreporting by country, where available.
Argentina: A retrospective review of medical records of deaths of women of childbearing age in 2014 estimated that maternal cause of death was omitted in 14.2% of maternal deaths and 33.3% of late maternal deaths.[6]
Austria: A study of maternal mortality in 1980-98 found 119 maternal deaths registered in the official statistics, while confidential inquiries found 191 maternal deaths, suggesting under-reporting of 38% (95% CI 31-45), with more indirect deaths under-reported (81%, 95% CI 64-92) than direct obstetrical deaths (28%, 95% CI 21-36).[7]
Brazil: A study estimating maternal death underreporting in 1988 in eight public maternity clinics in Rio de Janeiro found that the official death rate, based on maternal deaths as declared in death certificates, underreported by 60% compared to the corrected death rate.[8] A study of maternal deaths Paraná State in 1991-2005 based on Reproductive Age Mortality Surveys found that maternal mortality decreased by 26% over the 15 years, but that the level of underreporting remained the same over the period, ranging between 35.5% to 45.3%.[9]
Georgia: A national Reproductive Age Mortality Survey (RAMOS) conducted to examine maternal mortality in 2012 identified 23 maternal deaths, of which 14 (60.9%) were officially recognized by the Georgian CRVS, while all of the 36 pregnancy-related deaths identified were recorded in the CRVS.[10]
Ghana: A Reproductive Age Mortality Survey (RAMOS) conducted in Accra identified 179 maternal deaths in 2002, of which 101 (56%) were reported in the official statistics.[11]
India: A study of deaths among women of reproductive age in Vellore between 1999 and 2004 identified 28 maternal deaths, of which 14 were recorded in the official statistics, and only 10 were classified as maternal deaths, yielding a maternal mortality reporting rate of 36%.[12]
Indonesia: A study of 155 maternal deaths during 2003-2004 identified in the district hospitals of Pandeglang and Serang, in Banten Province, found that only 67 maternal deaths were recorded in the hospitals’ routine reports, suggesting that only 43% of maternal deaths were captured.[13] A later study in Banten Province of maternal deaths in 2016 estimated that 57% were captured by the district health office system.[14]
Italy: A study linking death registry and hospital discharge registry in 10 regions covering 77% of total national births from 2006 to 2012 identified 277 maternal deaths, and estimated that the official MMR underreports maternal mortality by 60.3%.[15]
Jamaica: A cross-sectional study to examine all maternal deaths occurring in 2008 from multiple data sources identified 50 maternal deaths, of which 10 (20%) were unregistered.[16]
Malawi: A prospective Reproductive Age Mortality Survey (RAMOS) conducted in Mangochi District in 2011-2012 identified 151 maternal deaths, of which 86 (57%) had been recorded in the official registration system, all of which were facility-based deaths.[17]
Mexico: An analysis of six studies examining underreporting of maternal deaths in Yucatan estimated that underreporting was 19% during 1997-2001, with rates varying between 10.5% and 28.6%.[18]
Morocco: A retrospective survey in Gharb Chrarda Bni Hssen region of deaths of women of reproductive age between January 1, 2013 and September 30, 2014 identified 69 maternal deaths, of which only 29 were registered in the maternal deaths surveillance system.[19]
Netherlands: A nationwide, retrospective study of maternal deaths during 1983-1992 estimated that the level of maternal mortality underreporting in The Netherlands was 26%.[20]
Norway: A study linking birth and cause of death registries supplemented with data from maternity clinics identified 26 maternal deaths in 2005-2009, of which only 14 (53.8%) were registered in the the official statistics.[21]
Papua New Guinea: A retrospective review of maternal deaths at Modilon General Hospital, Madang found that during 2008-2011 there was underreporting to the provincial health information office of maternal deaths (19/60, 31.7%) and also live births (2148/9098, 23.6%).[22]
Portugal: A study using multiple-capture methods from different data sources to examine maternal deaths between 2001 and 2006 estimated that maternal mortality was underestimated by 9%-26% in the official statistics.[23]
Sri Lanka: A study carried out in 1994-95 estimated that maternal deaths in the Western Province were 24% underreported.[24]
Suriname: A reproductive age mortality survey conducted between 2010 and 2014 estimated that 26% were underreported in vital registration data.[25]
Sweden: A national register-based study of deaths of women of reproductive age in 1988-2007 estimated that maternal mortality was 64% higher than reported to the World Health Organization.[26]
Switzerland: A study of Federal Statistical Office death certificates between 1995 and 2004 compared with maternal mortality cases from the archive of the Institute of Legal Medicine estimated that MMR was underreported by 20%.[27]
Taiwan: A census of all registered deaths among women of reproductive age in 1984-1988 found that only 53% of maternal deaths were correctly classified.[28] A nationwide data linkage study examining maternal deaths in 2004-2011 identified 236 maternal deaths, of which only 102 were reported in officially published mortality data, suggesting an underreporting rate of 57%.[29]
Tanzania: A study of the medical birth registry at Kilimanjaro Christian Medical Center in Moshi found that in 2000-2004 18 maternal deaths were recorded, however, hospital case records were found for 62 maternal deaths during the same period, thus only 29% of maternal deaths were entered into the registry.[30] A study carried out in 1995 in the main catchment area of Haydom Lutheran Hospital in rural Arusha identified 26 maternal deaths, of which 22 were recorded by the hospital, but only 2 were included in the official district statistics.[31]
Thailand: A study combining data from civil registration and inpatient diagnoses to identify maternal deaths in 2007-2014 estimated that the maternal mortality ratio (MMR) varied between 30.7-42.5, compared to the official MMR estimates of 8.9-23.3.[32]
USA: In the US, the National Vital Statistics System (NVSS) is the source of official maternal mortality estimates. However, it has been unable to supply accurate estimates of maternal mortality in the US due to problems in reporting and coding of data.[33] A study of maternal deaths occurring in Maryland during the years 1993 through 2000 found that 38% of maternal deaths were unreported on death certificates - half or more deaths were unreported for women who were undelivered at the time of death, experienced a fetal death or therapeutic abortion, died more than a week after delivery, or died as a result of a cardiovascular disorder.[34]
Zambia: A study comprising of hospital data and a sisterhood method survey in Kalabo District, rural western Zambia in 1994, found that the official number of maternal deaths was 13, but that further investigation revealed 28 maternal deaths in total, yielding a reporting rate of 46%.[35]
Parameters
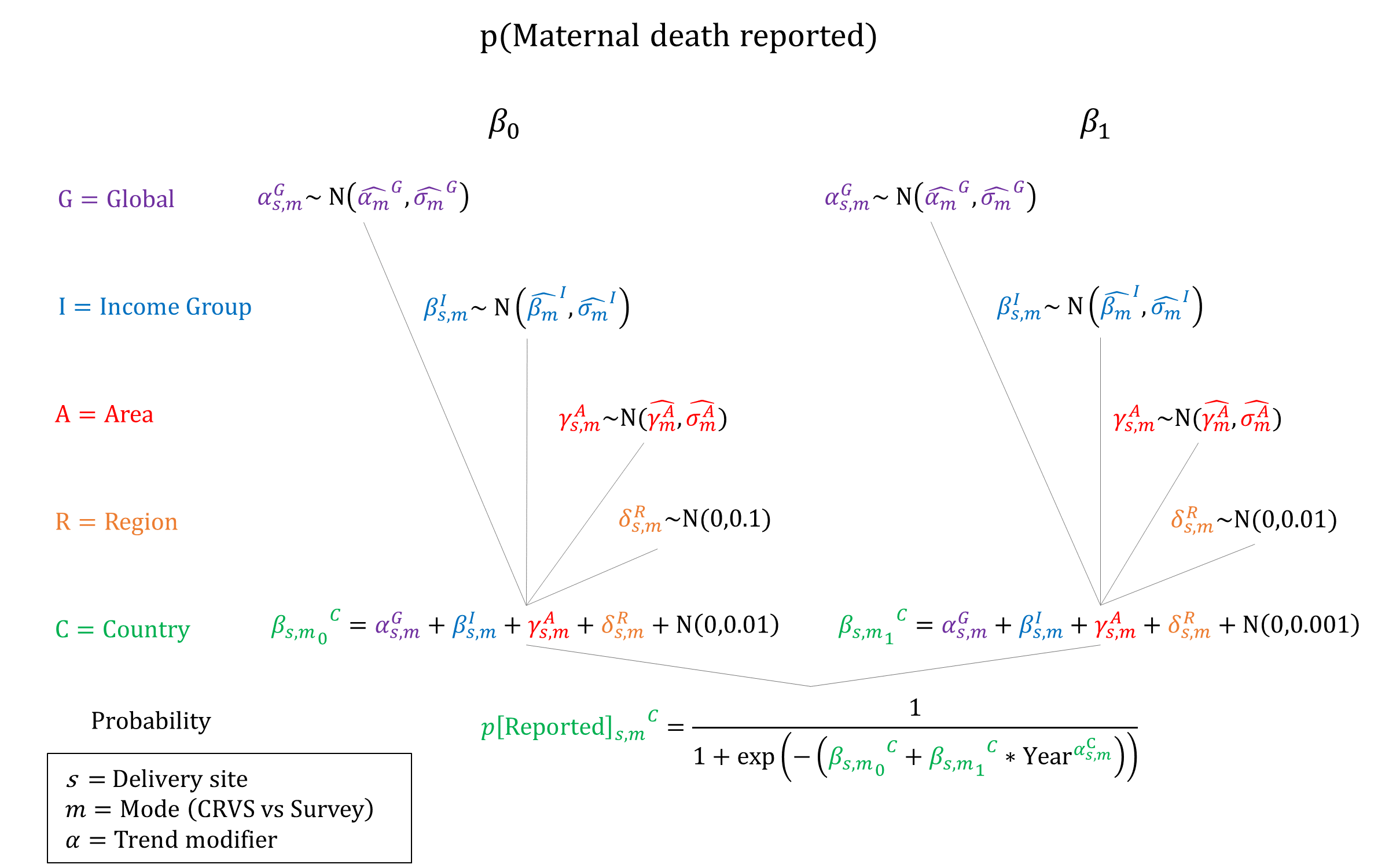
We used hierarchical logistic regression models to estimate the probability that maternal deaths are correctly classified and reported. We assume that reporting of maternal mortality is generally improving over time, so we constrain the year coefficient to be non-negative when sampling. Given the underreporting observed in institutions where record-keeping is theoretically in place, it would be expected that maternal deaths which occur in the community would be underreported to an even greater extent.[36] We therefore model differential probabilities of underreporting by delivery site and assume that the probability of a maternal death being accurately reported increases by site: Home < Home-SBA < non-EmOC < BEmOC < CEmOC. We also assume that survey data are more likely to report maternal deaths as surveys may be more representative of the population, and active case finding would be expected to yield more accurate estimates than passive death reporting. We therefore ensure that survey-based reporting probabilities are at least as high as the CRVS-based reporting probabilities.
Priors
Model Implementation
The (time-dependent) probabilities of underreporting are used to simulate whether each maternal death in the model is appropriately classified and recorded. Only recorded deaths in the model are scored against the calibration targets for maternal mortality, accounting for the reporting mode (CRVS vs survey) of each empirical estimate. For simplicity, we currently assume that underreporting of maternal deaths within each country varies by delivery site and reporting mode, but is non-differential by cause of death. However, this assumption could be relaxed in the future if more data on differential underreporting by cause of death become available.
References
- World Health Organization. Maternal mortality ratio (per 100 000 live births). The Global Health Observatory. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/26
- Wilmoth JR, Mizoguchi N, Oestergaard MZ, et al. A New Method for Deriving Global Estimates of Maternal Mortality. Stat Politics Policy 2012; 3(2): 2151-7509. DOI: https://doi.org/10.1515/2151-7509.1038
- United Nations Maternal Mortality Estimation Inter-Agency Group. Trends in maternal mortal-ity: 2000 to 2017. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva, World Health Organization, 2019. Available at www.who.int/reproductivehealth/publications/maternal−mortality−2017/en/
- Peterson E, Chou D, Moller AB, Gemmill A, Say L, Alkema L. Estimating maternal mortality using data from national civil registration vital statistics systems: A Bayesian hierarchical bivariate random walk model to estimate sensitivity and specificity of reporting. arxiv 2019: arXiv:1909.08578v1 https://arxiv.org/pdf/1909.08578.pdf
- Kassebaum NJ, Barber RM, Bhutta ZA, et al. Global, regional, and national levels of maternal mortality, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053): 1775-1812. DOI: https://doi.org/10.1016/s0140-6736(16)31470-2
- Abalos E, Duhau M, Escobar P, et al. [Omission of causes of maternal death in death certificates in Argentina: nationwide observational study Omissão do registro de causas maternas de morte na Argentina: estudo observacional de alcance nacional]. Rev Panam Salud Publica 2019; 43: e13. DOI: https://doi.org/10.26633/rpsp.2019.13
- Karimian-Teherani D, Haidinger G, Waldhoer T, Beck A, Vutuc C. Under-reporting of direct and indirect obstetrical deaths in Austria, 1980-98. Acta Obstet Gynecol Scand 2002; 81(4): 323-327. DOI: https://doi.org/10.1034/j.1600-0412.2002.810408.x
- Silva LK, Russomano FB. [Underreporting of maternal mortality in Rio de Janeiro, Brazil: comparison of 2 information systems]. Bol Oficina Sanit Panam 1996; 120(1): 36-43. PMID: https://pubmed.ncbi.nlm.nih.gov/8850128/
- Soares VM, de Azevedo EM, Watanabe TL. [Underreporting of maternal deaths in Paraná State, Brazil: 1991-2005]. Cad Saude Publica 2008; 24(10): 2418-2426. DOI: https://doi.org/10.1590/s0102-311x2008001000022
- Berdzuli N, Lomia N, Staff AC, Kereselidze M, Lazdane G, Jacobsen AF. Maternal Mortality in Georgia: Incidence, Causes and Level of Underreporting: A National Reproductive Age Mortality Study 2014. Int J Womens Health 2020; 12: 277-286. DOI: https://doi.org/10.2147/ijwh.s227349
- Zakariah AY, Alexander S, van Roosmalen J, Buekens P, Kwawukume EY, Frimpong P. Reproductive age mortality survey (RAMOS) in Accra, Ghana. Reprod Health 2009; 6: 7. DOI: https://doi.org/10.1186/1742-4755-6-7
- Kim SY, Rochat R, Rajaratnam A, Digirolamo A. Evaluating completeness of maternal mortality reporting in a rural health and social affairs unit in Vellore, India, 2004. J Biosoc Sci 2009; 41(2): 195-205. DOI: https://doi.org/10.1017/s0021932008003064
- Qomariyah SN, Bell JS, Pambudi ES, et al. A practical approach to identifying maternal deaths missed from routine hospital reports: lessons from Indonesia. Glob Health Action 2009; 2. DOI: https://doi.org/10.3402/gha.v2i0.1905
- Qomariyah SN, Sethi R, Izati YN, et al. No one data source captures all: A nested case-control study of the completeness of maternal death reporting in Banten Province, Indonesia. PLoS One 2020; 15(5): e0232080. DOI: https://doi.org/10.1371/journal.pone.0232080
- Donati S, Maraschini A, Lega I, et al. Maternal mortality in Italy: Results and perspectives of record-linkage analysis. Acta Obstet Gynecol Scand 2018; 97(11): 1317-1324. DOI: https://doi.org/10.1111/aogs.13415
- McCaw-Binns AM, Mullings JA, Yvette Holder. Vital registration and under-reporting of maternal mortality in Jamaica. Int J Gynaecol Obstet 2015; 128(1): 62-7. DOI: https://doi.org/10.1016/j.ijgo.2014.07.023
- Mgawadere F, Unkels R, Adegoke A, van den Broek N. Measuring maternal mortality using a Reproductive Age Mortality Study (RAMOS). BMC Pregnancy Childbirth 2016; 16(1): 291. DOI: https://doi.org/10.1186/s12884-016-1084-8
- Rodríguez-Angulo EM, Hoil-Santos JJ, Ojeda-Rodríguez R. Problems with Epidemiological Surveillance and Under-Reporting of Maternal Deaths in Yucatan, Mexico: An Analysis of Six Studies. In: Schwartz D. (eds) Maternal Death and Pregnancy-Related Morbidity Among Indigenous Women of Mexico and Central America. Global Maternal and Child Health (Medical, Anthropological, and Public Health Perspectives). 2018. Springer, Cham. DOI: https://doi.org/10.1007/978-3-319-71538-4_15
- Abouchadi S, Zhang WH, De Brouwere V. Underreporting of deaths in the maternal deaths surveillance system in one region of Morocco. PLoS One 2018; 13(1): e0188070. DOI: https://doi.org/10.1371/journal.pone.0188070
- Schuitemaker N, Van Roosmalen J, Dekker G, Van Dongen P, Van Geijn H, Gravenhorst JB. Underreporting of maternal mortality in The Netherlands. Obstet Gynecol 1997; 90(1): 78-82. DOI: https://doi.org/10.1016/s0029-7844(97)00128-2
- Vangen S, Ellingsen L, Andersgaard AB, et al. [Maternal deaths in Norway 2005‐2009]. Tidsskr Nor Laegeforen 2014; 134: 836-9. DOI: https://doi.org/10.4045/tidsskr.13.0203
- Bolnga JW, Hamura NN, Umbers AJ, Rogerson SJ, Unger HW. Insights into maternal mortality in Madang Province, Papua New Guinea. Int J Gynaecol Obstet 2014; 124(2): 123-7. DOI: https://doi.org/10.1016/j.ijgo.2013.08.012
- Gomes MC, Ventura MT, Nunes RS. How many maternal deaths are there in Portugal? J Matern Fetal Neonatal Med 2012; 25(10): 1975-9. DOI: https://doi.org/10.3109/14767058.2012.668587
- Bandhutilaka THC. Epidemiology of Maternal Mortality in Sri Lanka. 1996. MD thesis. Colombo: Post Graduate Institute of Medicine, University of Colombo. http://librepository.pgim.cmb.ac.lk/handle/1/968
- Kodan LR, Verschueren KJC, van Roosmalen J, Kanhai HHH, Bloemenkamp KWM. Maternal mortality audit in Suriname between 2010 and 2014, a reproductive age mortality survey. BMC Pregnancy Childbirth 2017; 17(1): 275. DOI: https://doi.org/10.1186/s12884-017-1466-6
- Esscher A, Högberg U, Haglund B, Essën B. Maternal mortality in Sweden 1988-2007: more deaths than officially reported. Acta Obstet Gynecol Scand 2013; 92(1): 40-46. DOI: https://doi.org/10.1111/aogs.12037
- Fässler M, Zimmermann R, QuackLötscher KC. Maternal mortality in Switzerland 1995-2004. Swiss Med Wkly 2010; 140(1-2): 25-30. Available at: https://www.zora.uzh.ch/id/eprint/44439/1/Faessler_smw-12768.pdf
- Kao S, Chen LM, Shi L, Weinrich MC. Underreporting and misclassification of maternal mortality in Taiwan. Acta Obstet Gynecol Scand 1997; 76(7): 629-636. DOI: https://doi.org/10.3109/00016349709024602
- Wu TP, Liang FW, Huang YL, Chen LH, Lu TH. Maternal Mortality in Taiwan: A Nationwide Data Linkage Study. PLoS One 2015; 10(8): e0132547. DOI: https://dx.doi.org/10.1371%2Fjournal.pone.0132547
- Bergsjø P, Vangen S, Lie RT, Lyatuu R, Lie-Nielsen E, Oneko O. Recording of maternal deaths in an East African university hospital. Acta Obstet Gynecol Scand. 2010; 89(6): 789-793. DOI: https://doi.org/10.3109/00016341003801664
- Olsen BE, Hinderaker SG, Lie RT, Bergsjø P, Gasheka P, Kvåle G. Maternal mortality in northern rural Tanzania: assessing the completeness of various information sources. Acta Obstet Gynecol Scand 2002; 81(4): 301-307. DOI: https://doi.org/10.1034/j.1600-0412.2002.810404.x
- Chandoevwit W, Phatchana P, Sirigomon K, Ieawsuwan K, Thungthong J, Ruangdej S. Improving the measurement of maternal mortality in Thailand using multiple data sources. Popul Health Metr 2016; 14: 16. DOI: https://doi.org/10.1186/s12963-016-0087-z
- MacDorman MF, Declercq E. The failure of United States maternal mortality reporting and its impact on women’s lives. Birth 2018; 45(2): 105-108. DOI: https://doi.org/10.1111/birt.12333
- Horon IL. Underreporting of Maternal Deaths on Death Certificates and the Magnitude of the Problem of Maternal Mortality. Am J Public Health 2005; 95(3): 478-482. DOI: https://dx.doi.org/10.2105%2FAJPH.2004.040063
- Vork FC, Kyanamina S, van Roosmalen J. Maternal mortality in rural Zambia. Acta Obstet Gynecol Scand 1997; 76(7): 646-650. DOI: https://doi.org/10.3109/00016349709024604
- Cross S, Bell JS, Graham WJ. What you count is what you target: the implications of maternal death classification for tracking progress towards reducing maternal mortality in developing countries. Bull World Health Organ 2010; 88(2): 147–153. DOI: https://dx.doi.org/10.2471%2FBLT.09.063537
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu