Obstructed Labor
Model Inputs \(\rightarrow\) Obstetric Complications \(\rightarrow\) Obstructed Labor
Overview
Labor is considered obstructed when the presenting part of the fetus cannot progress into the birth canal, despite strong uterine contractions.[1] It usually arises from mechanical factors of maternal origin (e.g. small pelvis, pelvic contractures, nongynecoid pelvis, etc.) or of fetal origin (abnormal presentation and/or position, large fetus [macrosomia], abnormally large fetal parts [e.g. hydrocephalus, tumors], etc.).[2] Obstruction can occur at the pelvic inlet, in the pelvic cavity or at the pelvic outlet. If neglected, it can result in endometritis, obstetric fistula (rectovaginal or vesicovaginal), and ruptured uterus with consequent hemorrhage, shock or death. It also leads to significant perinatal morbidity and mortality. Women who are malnourished, marry young, or engage in childbearing at an early age before the pelvis has reached adult proportions, are at high risk for obstructed labor. However, there is no evidence to show that interventions aimed at providing adequate childhood nutrition or delayed childbearing prevents obstructed labor.[3]
Data
Incidence
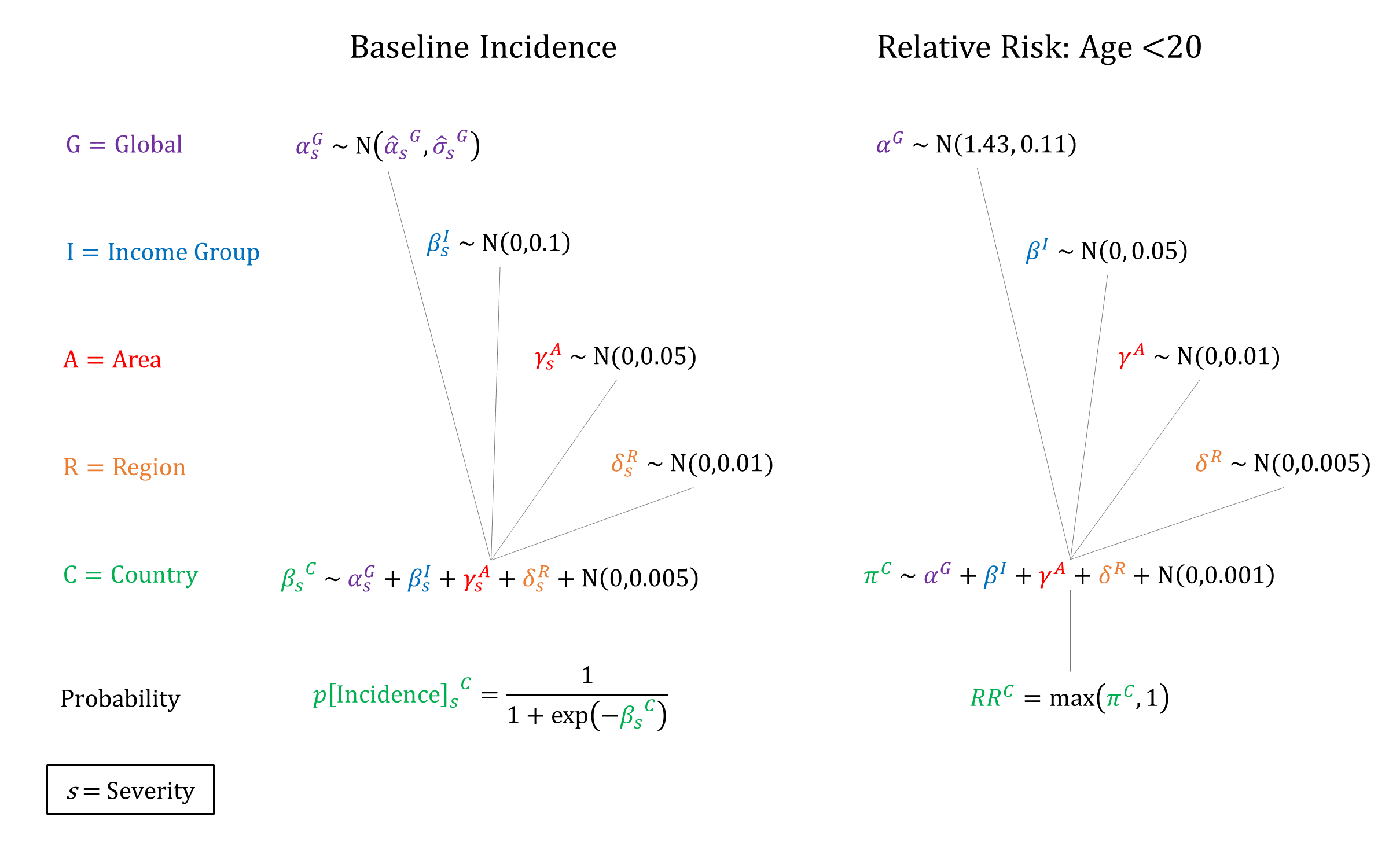
Obstructed labor is estimated to affect 4.6% of live births, although it varies considerably among different regions of the world.[1,4] A review of studies from 1960-2003 reports incidence estimates ranging from 1% to 7%.[5] According to Filippi 2016,[6] an unpublished systematic review by Adler and others yielded only 16 published population-based studies of obstructed and prolonged labor worldwide since 2000. The studies could not be combined through meta-analysis to obtain a global prevalence because of high heterogeneity, which was largely attributed to differences in case definitions. However, the median prevalence was estimated to be 1.9 per 100 deliveries for obstructed labor, and 8.7 per 100 deliveries for combined obstructed and prolonged labor. There is evidence that a higher incidence of obstructed labor is associated with younger age groups - Kabakyenga 2011[7] estimated an odds ratio of obstructed labor of 1.43 (95% CI 1.23-1.67) for women between the ages of 15-19, compared to older women.
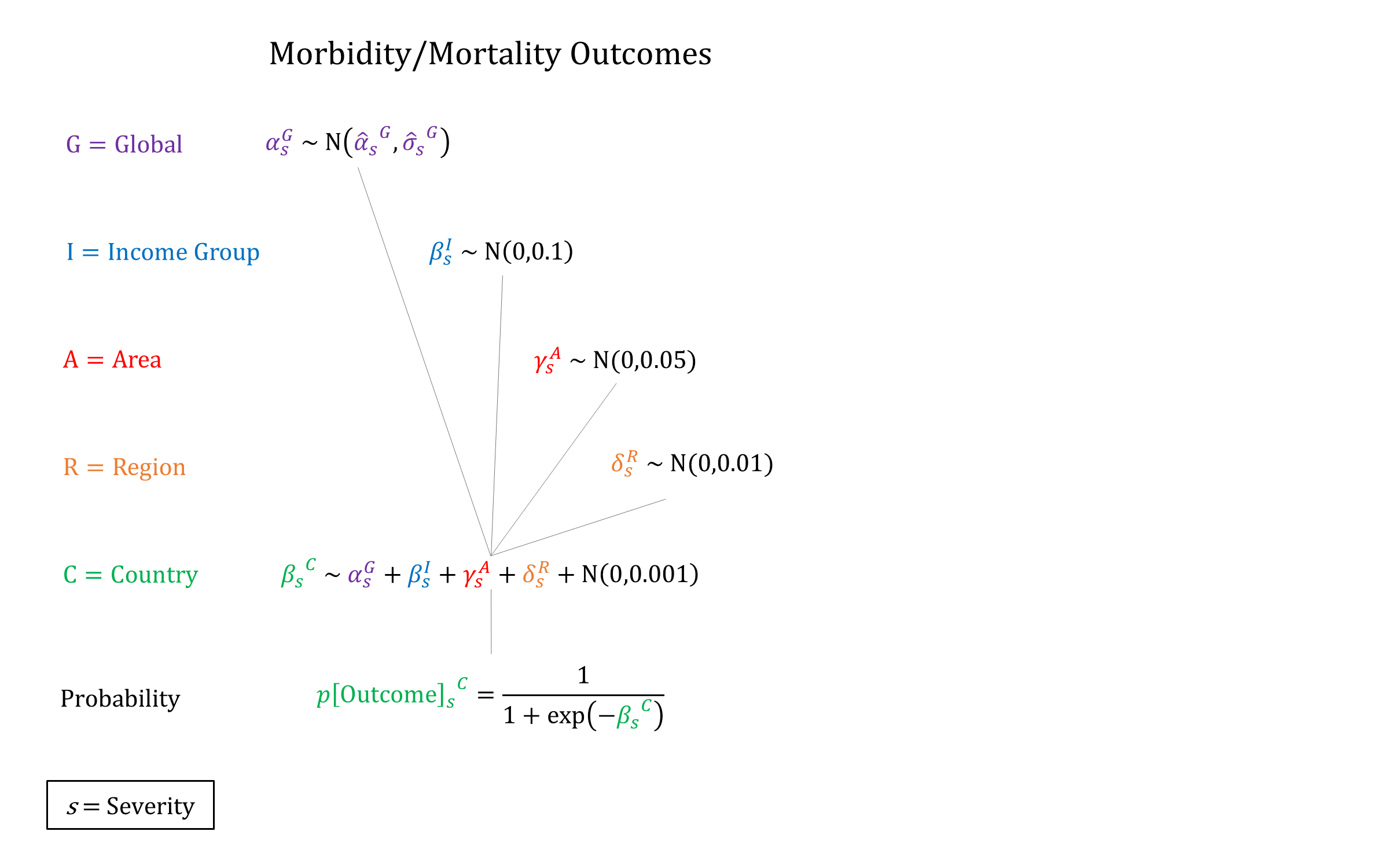
Morbidity/Mortality
A review conducted by the Disease Control Priorities Project (DCP2) reported an average case fatality rate of 0.7% for obstructed labor,[8] while a review of studies from 1960-2003 finds an average mortality risk of 5.5%, ranging from 0.8% to 16.6%.[5] In addition to mortality, there is also the risk of fistula from obstructed labor. As a result of the severe delay in delivery and continuous pressure of the fetal head on maternal tissues, blood flow is blocked resulting in necrosis. This leaves abnormal gaps (or communications) between the vagina and bladder or rectum, allowing urine or stool to pass continuously through the vagina.[6] Obstetric fistula was estimated to occur in 2.15% of neglected obstructed labor cases,[1] while a review of studies from 1960-2003 finds an average risk of fistula from obstructed labor of 3.4%, ranging from 0.4% to 6.6%.[5]
In addition, obstructed labor is linked with increased rates of stillbirth, especially for women who develop fistula as a result of obstructed labor. Estimates of the proportion of women with obstetric fistula who also experience stillbirth range from 32.3% to 100%, with estimates from the largest studies around 92%.[9]
Parameters
We used a hierarchical logistic regression model for the incidence of obstructed labor and model 2 levels of severity: moderate and severe obstructed labor. We also account for higher risk of obstructed labor for women less than 20 years old. Conditional on developing obstructed labor we model risks of mortality, obstetric fistula, and stillbirth, with higher risks for severe vs moderate obstructed labor. To account for the relationship between obstetric fistula and stillbirth we model a higher risk of stillbirth for women who experience fistula.
Priors
Note: For stillbirth risk, ‘Severe’ denotes that the woman experienced an obstetric fistula.Model Implementation
At the time of delivery, the incidence and outcomes of obstructed labor are simulated, together with the availability and efficacy of interventions that modify the ‘natural history’ probabilities.
References
- Dolea C, AbouZahr C. Global Burden of Obstructed Labour in the Year 2000. Evidence and information for policy (EIP). Global Burden of Disease Working Paper, 2003. Available at: https://www.who.int/healthinfo/statistics/bod_obstructedlabour.pdf
- Lawson JB. Obstructed Labour. BJOG 1965; 72(6): 877-880. DOI: https://doi.org/10.1111/j.1471-0528.1965.tb01506.x
- Tsu VD, Coffey PS. New and underutilised technologies to reduce maternal mortality and morbidity: what progress have we made since Bellagio 2003? BJOG 2009; 116(2): 247-56. DOI: https://doi.org/10.1111/j.1471-0528.2008.02046.x
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet 2006; 367(9516): 1066-1074. DOI: https://doi.org/10.1016/s0140-6736(06)68397-9
- Wall LL. A framework for analyzing the determinants of obstetric fistula formation. Stud Fam Plann 2012; 43(4): 255-72. DOI: https://doi.org/10.1111/j.1728-4465.2012.00325.x
- Filippi V, Chou D, Ronsmans C, Graham W, Say L. Chapter 3. Levels and causes of maternal mortality and morbidity. In: Black RE, Laxminarayan L, Walker N, Temmerman M, eds. Disease control priorities 3rd edn. Volume 2. Reproductive, maternal, newborn and child health. Washington, DC: World Bank, 2016. Available at: https://www.ncbi.nlm.nih.gov/books/NBK361917/
- Kabakyenga JK, Östergren PO, Turyakira E, Mukasa PE, Pettersson KO. Individual and health facility factors and the risk for obstructed labour and its adverse outcomes in south-western Uganda. BMC Pregnancy Childbirth 2011; 11: 73. DOI: https://doi.org/10.1186/1471-2393-11-73
- Graham WJ, Cairns J, Bhattacharya S, et al. Maternal and Perinatal Conditions. In: Jamison DT, Breman JG, Measham AR, et al, eds. Disease Control Priorities in Developing Countries. 2nd edition. Washington (DC): World Bank; 2006. Available at: https://www.ncbi.nlm.nih.gov/books/NBK11742/
- Cowgill KD, Bishop J, Norgaard AK, Rubens CE, Gravett MG. Obstetric fistula in low-resource countries: an under-valued and under-studied problem–systematic review of its incidence, prevalence, and association with stillbirth. BMC Pregnancy Childbirth 2015; 15: 193. DOI: https://doi.org/10.1186/s12884-015-0592-2
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu