Indirect Maternal Deaths
Model Inputs \(\rightarrow\) Obstetric Complications \(\rightarrow\) Indirect Maternal Deaths
Overview
An indirect maternal death is defined as a “maternal death resulting from previous existing disease or disease that developed during pregnancy and which was not due to direct obstetric causes, but which was aggravated by physiologic effects of pregnancy”.[1] Indirect maternal deaths outnumber direct maternal deaths due to obstetric causes in many high-income countries, and have grown substantially as a proportion of all maternal deaths in low- and middle-income countries.[2] It is important to distinguish between direct and indirect maternal deaths when planning and evaluating interventions to improve maternal health, as failure to differentiate between causes may lead to unrealistic expectations about the effect of an intervention on total maternal deaths, or misallocation of resources away from major causes of death.[3]
Data
We obtained data on reported deaths from all causes for women ages 15-49 years from the WHO Mortality Database, a compilation of mortality data by age, sex, and cause of death, as reported annually by countries from their civil registration systems.[4] We restricted the data to observations where the reported causes of maternal death summed to the total number of reported maternal deaths, yielding 1730 estimates from 115 countries between 1994-2018. We used these data to set priors on the proportion of all-cause mortality due to direct maternal deaths (i.e. due to ICD-10 codes corresponding to causes of death explicitly included in the model - see Maternal Death ICD Codes). We use these estimates to ‘back out’ the risk of direct maternal death for women ages 15-49 from the lifetables used in the model, leaving the risk of indirect maternal deaths as part of the background mortality rates included in the model.
Parameters
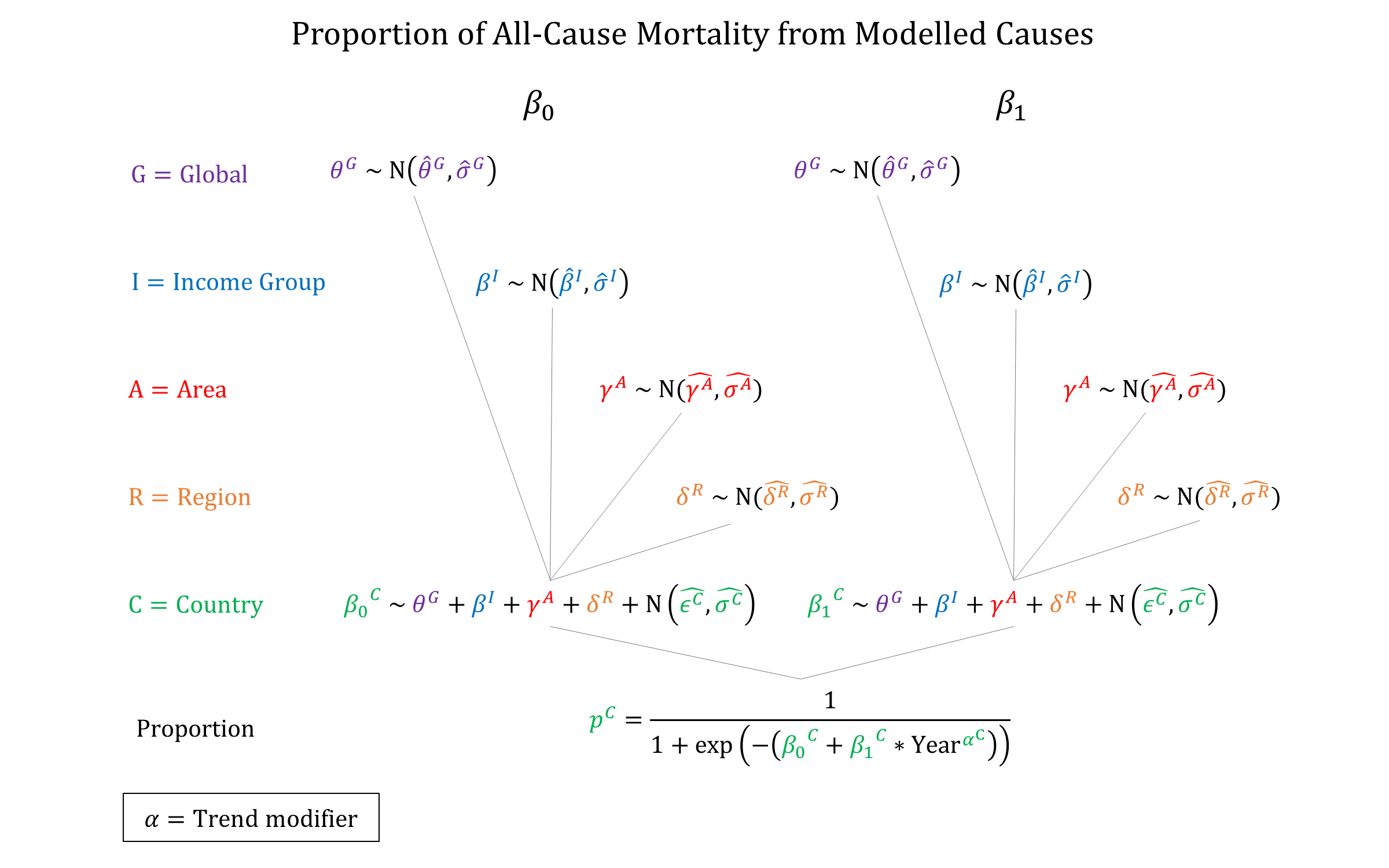
We used a hierarchical logistic regression model to model the proportion of total female mortality (15-49) from direct maternal causes included in the model. This approach allows us to account for differences in the risk of indirect maternal deaths in different settings.
Priors
Model Implementation
We use the modelled proportion of female deaths already explicitly included in the model to proportionally lower the all-cause mortality rates from the lifetables for women ages 15-49. If a woman dies from this adjusted background mortality risk during or within 2 months of pregnancy it is considered an indirect maternal death if it is not due to incidental/accidental causes.
References
- World Health Organization. The WHO application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: ICD-MM, Geneva: World Health Organization, 2012. Available at: https://www.who.int/reproductivehealth/publications/monitoring/9789241548458/en/
- Nair M, Nelson-Piercy C, Knight M. Indirect maternal deaths: UK and global perspectives. Obstet Med 2017; 10(1): 10-15. DOI: https://dx.doi.org/10.1177%2F1753495X16689444
- Cross S, Bell JS, Graham WJ. What you count is what you target: the implications of maternal death classification for tracking progress towards reducing maternal mortality in developing countries. Bull World Health Organ 2010; 88(2): 147-53. DOI: https://doi.org/10.2471/blt.09.063537
- World Health Organization. WHO Mortality Database - Last updated: 15 December 2019. Available at: https://www.who.int/healthinfo/mortality_data/en/
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu