Partograph
Model Inputs \(\rightarrow\) Clinical Interventions \(\rightarrow\) Partograph
Overview
The partograph graphically represents key events in labor and provides an early warning system. The World Health Organization partographs are the best known partographs in low resource settings. Experiences with World Health Organization and other types of partographs in low resource settings suggest that when used with defined management protocols, this inexpensive tool can effectively monitor labor and prevent obstructed labor.[1]
Data
A WHO trial in 1987 in South-East Asia involving 35,484 women found that partograph use reduced by half both prolonged labor (from 6.4% to 3.4%), and the proportion of labors requiring augmentation (from 20.7% to 9.1%).[2] Similar reductions were found in a prospective study of 1000 women in Karachi, Pakistan. Before introduction of the partograph only 80.8% of women delivered within 12 hours, compared to 91.6% after the partograph was introduced.[3]
However, a recent Cochrane review concluded that there was no clear evidence that partographs improve outcomes (e.g. c-section rate, oxytocin augmentation), or that one type of partograph is greatly superior to another.[4] Nevertheless, the review acknowledges that partograph use is widespread in both low-income and high-income settings, with reported quality of care benefits,[5] and that evidence from non-randomized trials report potential benefits of partograph use.[5,6,7] Given these findings, we set wide priors for the efficacy of partographs in reducing the incidence of obstructed labor.
Parameters
We model the use and efficacy of partographs, and assume that use increases by delivery site and income group, and that it is not available at home. We assume that partograph use increases over time and so constrain the year coefficient to be non-negative when sampling. We assume that the efficacy of partographs on reducing obstructed labor incidence is non-differential by severity.
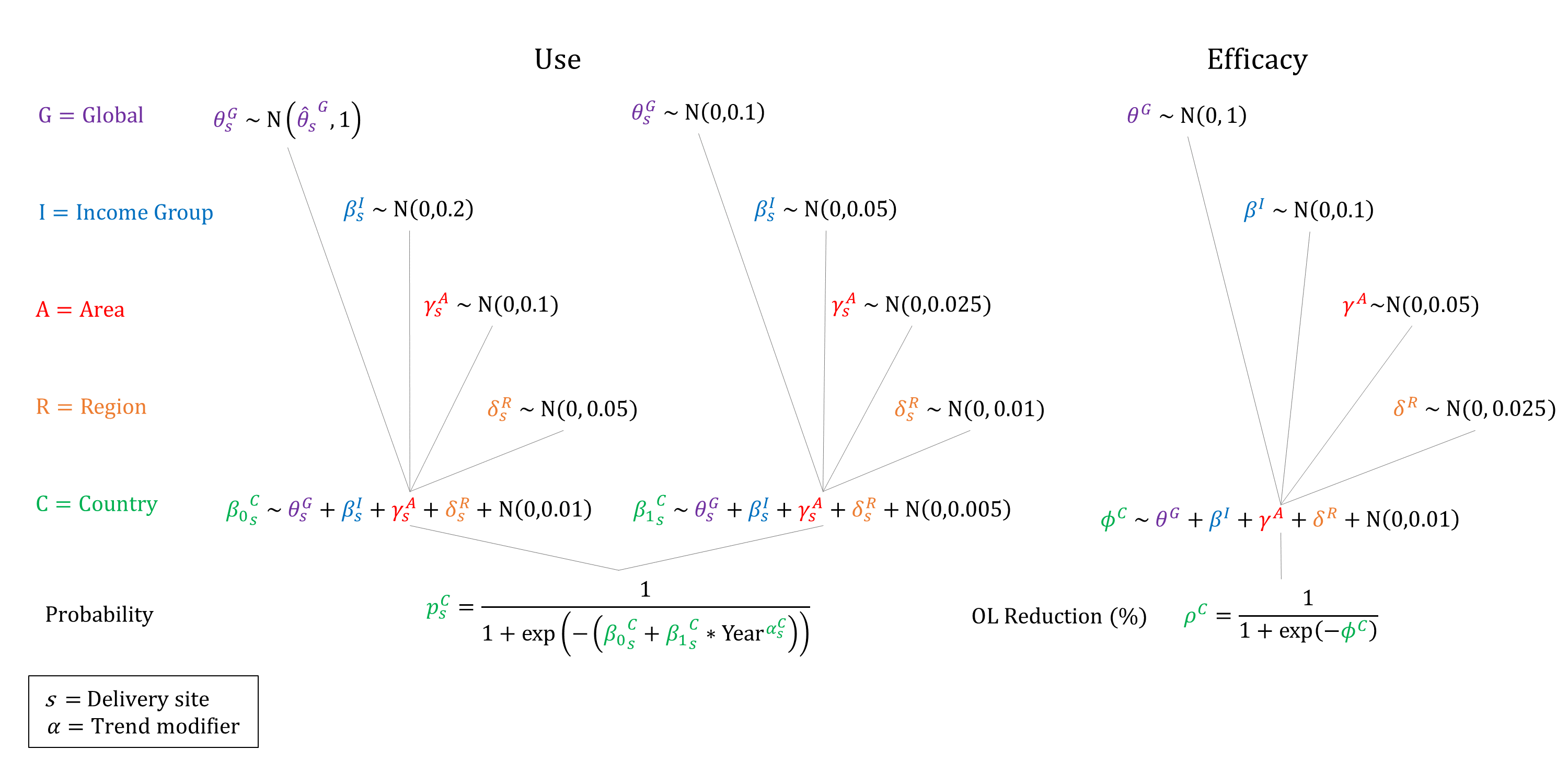
Priors
Model Implementation
Conditional on the site of delivery we simulate the probability that a partograph will be used and its efficacy on reducing the incidence of obstructed labor.
References
- Mathai M. The partograph for the prevention of obstructed labor. Clin Obstet Gynecol 2009; 52(2): 256-69. DOI: https://doi.org/10.1097/grf.0b013e3181a4f163
- World Health Organization Maternal Health and Safe Motherhood Programme. World Health Organization partograph in management of labour. Lancet. 1994; 343(8910): 1399-404. PMID: https://pubmed.ncbi.nlm.nih.gov/7910888/
- Javed I, Bhutta S, Shoaib T. Role of partogram in preventing prolonged labour. J Pak Med Assoc 2007; 57(8): 408-11. PMID: https://pubmed.ncbi.nlm.nih.gov/17902525/
- Lavender T, Cuthbert A, Smyth RM. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev 2018; 8(8): CD005461. DOI: https://doi.org/10.1002/14651858.cd005461.pub5
- Bedwell C, Levin K, Pett C, Lavender T. A realist review of the partograph: when and how does it work for labour monitoring? BMC Pregnancy Childbirth 2017; 17: 31. DOI: https://doi.org/10.1186/s12884-016-1213-4
- Bosse G, Massawe S, Jahn A. The partograph in daily practice: It’s quality that matters. Int J Gynaecol Obstet 2002; 77(3): 243–4. DOI: https://doi.org/10.1016/s0020-7292(02)00004-8
- Fawole AO, Hunyinbo KI, Adekanle DA. Knowledge and utilization of the partograph among obstetric care givers in South West Nigeria. Afr J Reprod Health 2008; 12(1): 22–9. PMID: https://pubmed.ncbi.nlm.nih.gov/20695151/
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu