Hemorrhage Treatment
Model Inputs \(\rightarrow\) Clinical Interventions \(\rightarrow\) Hemorrhage Treatment
Overview
Treatment options for hemorrhage include uterotonic drugs to increase muscle contractions (such as oxytocin and misoprostol) and surgical techniques (such as tying off or blocking the uterine artery) and blood transfusion.[1] In addition, although it is not a uterotonic, tranexamic acid may reduce mortality due to bleeding from postpartum hemorrhage when given within the first three hours and may be considered as an adjuvant therapy.[2] For women with severe, intractable hemorrhage hysterectomy provides a definitive treatment.[2] While hysterectomy is often a last resort in high-income settings, in settings where many women are anaemic and blood supplies are limited, such as Africa and Asia, hysterectomy is often used as an early intervention to prevent death from exsanguination.[3]
Data
Oxytocin is the most effective treatment for PPH, even if already used for labor induction or augmentation or as part of active management,[2] and is strongly recommended by the WHO.[4] Uterotonics can also be provided for women delivering at home. For example, a study in Indonesia found that in the majority of the PPH cases included in the study, uterotonic medication was started at home by the healthcare provider - in most cases, an IV line was established and the first dose of intramuscular oxytocin was provided before transportation to the third level of care.[5] While uterotonics are often widely available, surgical intervention and blood transfusion are less available. For example, data from the India District Level Household Survey 2007-2008 reported that that 9.1% of community health centers have a blood storage facility.[6]
An international randomised controlled trial of tranexamic acid found that death due to bleeding was significantly reduced in women given tranexamic acid (1.5% vs 1.9% in the placebo group, RR 0.81, 95% CI 0.65–1.00), especially for women given treatment within 3 hours of giving birth (1.2% in the tranexamic acid group vs 1.7% in the placebo group, RR 0.69, 95% CI 0.52–0.91).[3]
Parameters
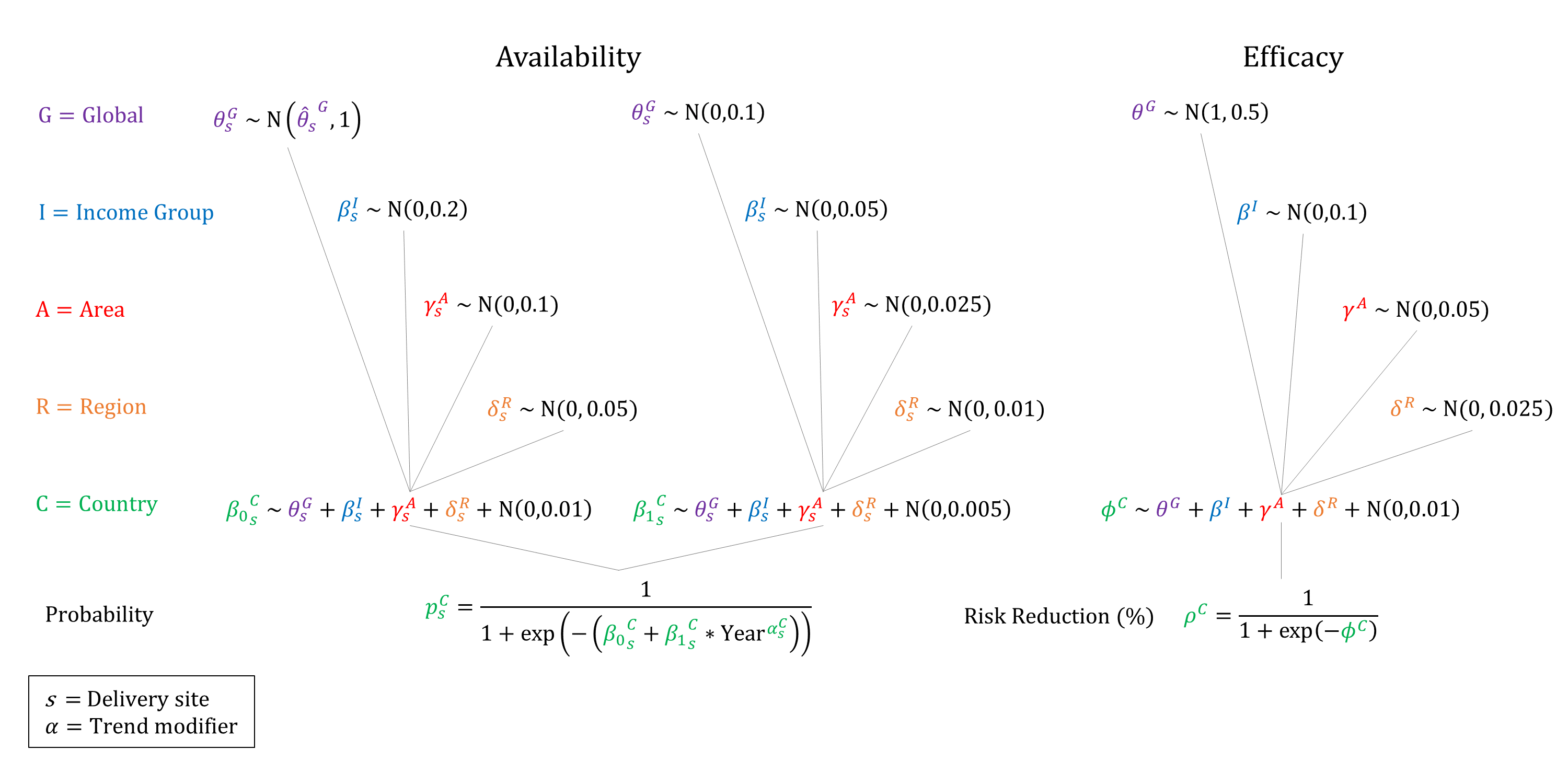
For women with PPH, we model the availability and efficacy of hemorrhage treatment, conditional on delivery site. We assume that the availability of treatment increases by site and income group, and that while uterotonics may be delivered at Home-SBA, surgical management and transfusion is not available at home. We therefore assume that ‘severe’ and ‘most severe’ PPH require surgical intervention and can only be treated at CEmOC facilities. We assume that treatment availability increases over time and so constrain the year coefficient to be non-negative when sampling. We assume that the efficacy of treatment is non-differential by severity, and apply the same risk reduction for all mortality and morbidity outcomes. We set efficacy priors centered near 75%.
Priors
Model Implementation
Conditional on the delivery site we simulate the probabilities that treatment will be available and the efficacy of treatment on hemorrhage outcomes, accounting for quality of care. We assume that women with ‘most severe’ PPH can only be treated at CEmOC facilities and undergo a hysterectomy.
References
- Mousa HA, Blum J, Abou El Senoun G, Shakur H, Alfirevic Z. Treatment for primary postpartum haemorrhage. Cochrane Database Syst Rev 2014; 2: CD003249. DOI: https://doi.org/10.1002/14651858.cd003249.pub3
- Evensen A, Anderson JM, Fontaine P. Postpartum Hemorrhage: Prevention and Treatment. Am Fam Physician 2017; 95(7): 442-449. Available at: https://www.aafp.org/afp/2017/0401/p442.html
- WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet 2017; 389(10084): 2105-2116. DOI: https://doi.org/10.1016/s0140-6736(17)30638-4
- World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. 2012. Available at: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/9789241548502/en/
- Rosales A, Sulistyo S, Miko O, et al. Recognition of and care-seeking for maternal and newborn complications in Jayawijaya district, Papua province, Indonesia: a qualitative study. J Health Popul Nutr 2017; 36(Suppl1): 44. DOI: https://doi.org/10.1186/s41043-017-0122-0
- International Institute for Population Sciences. India District Level Household Survey 2007-2008. Mumbai, India: International Institute for Population Sciences; 2010. Available: http://rchiips.org/PRCH-3.html.
GMatH (Global Maternal Health) Model - Last updated: 28 November 2022
© Copyright 2020-2022 Zachary J. Ward
zward@hsph.harvard.edu